When Katie Fox walked into
Wellstar North Fulton Medical Center
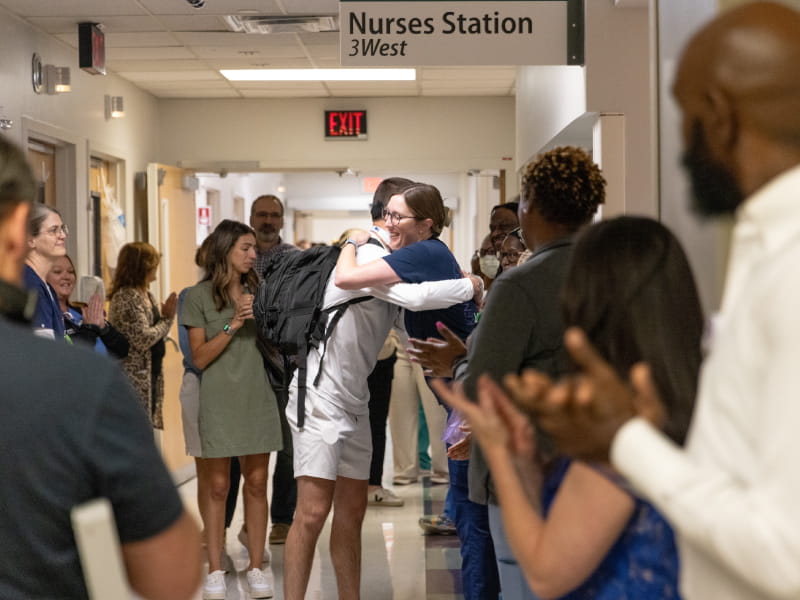
nearly a year after her devastating car crash, she felt the weight of the full-circle moment.
Across the atrium stood the people who had helped save her life—doctors, nurses and first responders who had seen her at her most critical and were now seeing her fully herself.
Katie had no memory of the three weeks she spent at Wellstar North Fulton—but her family remembered everything. So did her care team, who had been there through emergency surgery, intensive care, multiple procedures and round-the-clock support.
Now, just 10 months later, Katie was back—walking, smiling and thriving—thanks to her own resilience, an unwavering support system and the highly skilled trauma team at Wellstar North Fulton.
The crash that changed everything
Katie was involved in a car accident on Georgia State Route 400 that sent her to Wellstar North Fulton in critical condition. She had suffered a traumatic brain injury, a lacerated spleen and multiple fractures—including to her ribs, left ankle and pelvis.
Wellstar North Fulton is specially equipped to care for patients like Katie. Designated a
Level II Trauma Center
by the Georgia Department of Public Health and American College of Surgeons, the hospital serves the Northeast Atlanta community with immediate surgical intervention, 24/7 trauma coverage and seamless coordination across specialties.
“When they first brought her in, she was obviously severely injured in multiple areas,” said
Dr. Stephen McBride,
a trauma and general surgeon at Wellstar. “She had a large scalp laceration that was bleeding. We also noticed significant internal bleeding from her spleen and multiple pelvic fractures.”
A CT scan revealed a buildup of fluid in Katie’s abdomen, likely blood. She was taken straight to the operating room for what Dr. McBride called a “damage control operation.”
“We opened her abdomen and took her spleen out, which was very severely injured,” he said. “Then it was a matter of getting her stable.”
The surgery was a success—but it was only the beginning. Katie spent the next 10 days on a ventilator in the ICU. During her 19-day stay, she underwent multiple procedures and received care from a collaborative, multidisciplinary team: trauma surgery, neurosurgery, orthopedics, therapy and nursing.
Finding clarity and compassion
Katie’s parents, Mary Lou and Jeff Fox, flew in from Virginia as soon as they learned about the accident—first alerted by a message from Katie’s smart watch.
Jeff recalls speaking with Dr. McBride before takeoff and again after landing. “He was keeping us updated with what was going on with Katie from the start,” he said.
At Wellstar North Fulton, the couple were met with empathy and reassurance under unthinkable circumstances.
“When we got in, they took us straight to Katie,” Jeff said. “I didn’t know what to expect. It was probably the hardest moment of my life—seeing my baby there.”
Katie was unconscious and on a ventilator, but her care team made space for both expert treatment and emotional support. Jeff remembers nurses and even the front desk team checking on them constantly—offering updates, comfort and prayer.
One quiet act of compassion stood out. “The night of Katie’s accident, we stayed in the room with her,” said Mary Lou. “But her boyfriend, her roommate and a friend stayed in the waiting room. We don’t know who it was, but one of the caregivers placed blankets over each of them while they slept.”
That moment—and so many others—confirmed they were in the right place. “I’ll never forget the love and care we received,” Mary Lou said.
Milestones that mattered
Amid the uncertainty of Katie’s condition, small moments brought glimmers of hope. From the way her vital signs responded to blood transfusions to the subtle movements that followed, each step forward reminded her care team and loved ones that she was still fighting.
One emotional turning point came when her boyfriend, Will Henley, sat with her for the first time since the accident.
“I started talking to her about my day, and she opened her eyes,” he said. “I immediately asked her nurse if she had done that for anyone else and she said no. It wasn't much, but it was all I needed to keep my faith.”
Even while unconscious, Katie’s team spoke to her directly. “That was very special,” Mary Lou said. “Her doctors always included her in conversations about her care.”
Wellstar Neurosurgeon Dr. Benjamin Zussman
became one of her biggest cheerleaders, celebrating every sign of progress.
“We were exhausted and reality was beginning to set in,” Mary Lou said. “His enthusiasm helped us so much.”
Slowly, Katie began following motion with her eyes. At one point, she mouthed lyrics to Taylor Swift songs when Will played them at her bedside.
Throughout her time in the ICU, Katie’s care extended far beyond medicine. Nurses Sarah Kozarcanin and Sydney Dawson spent hours gently washing Katie’s hair to carefully clean around her head wound.
“That was an act of love that was above and beyond to me,” Jeff recalled.
Care united by purpose
As Katie came off the ventilator and slowly regained strength, the therapy team stepped in to help her sit up and begin basic movements. Her parents saw how seamlessly everyone worked together.
Dr. McBride credits the hospital’s collaborative approach. “Our hospital does a great job having the appropriate consultants available—neurosurgeons for severe brain injury, orthopedic surgeons for severe musculoskeletal injury and, of course, trauma surgeons, physician assistants (PA) and nurse practitioners who care for our patients from start to finish,” he said. “And then there are the therapists, social workers and case managers—all of whom play a key role in recovery.”
Jeff especially appreciated how the team included him and Mary Lou in the process. “Every morning, all the departments involved in Katie’s care would meet,” he said. “They’d always ask, ‘Do you want to join us?’ They valued our input.”
Looking ahead with hope
Katie was discharged and transferred to inpatient rehabilitation, where her memory gradually returned. She and her family celebrated every milestone—especially the day she no longer needed a wheelchair.
“Walking again felt like I gained a lot of freedom back,” Katie said.
Just over four months later, she was back to work, driving and living independently. She credits her recovery to her care team, family and Will—now her fiancé.
“His unwavering support and love during those months showed me that he would be the perfect husband,” Katie said. “If he could be my anchor and love me through that, I knew he would love me through anything.”
Katie also discovered a new sense of purpose. “This confirmed every desire I had to become a PA,” she said. “I think it will give me a different connection to patients.”
In the months after her discharge, Katie returned to the ICU several times to meet the people she had heard so much about—but hadn’t been able to remember.
“Each time we visited, they’d say, ’You can go in the back way—you’re like family now,’” Mary Lou said with a smile.
For Katie’s family, the hospital’s trauma survivor reception brought closure and gratitude. “We had always wanted to meet the first responders who got her out of the car and to the hospital,” said Jeff. "It was awesome that we finally had that opportunity.”
“Seeing good outcomes is the best part of my job, without a doubt,” said Dr. McBride, who attended the event. “For someone like Katie—young, healthy and just in the wrong place at the wrong time—it’s rewarding to see her get her life back.”
Katie’s story is a testament to the power of expert trauma care, teamwork and hope.
“I will forever be grateful for the care, kindness and love the people at Wellstar North Fulton gave my family and me,” Katie said. “We will never forget any of them.”
Learn more about trauma services at Wellstar.