
PhyllisCare
From screening to surgery with the Wellstar STAT Clinic for Lung Cancer
Published on May 27, 2025
Last updated 01:33 PM May 27, 2025


Cancers are so insidious. You’re not going to just go, 'Gee, I don’t feel good; it must be cancer.' There’s no big warning signs until it’s serious. Early detection is absolutely our best weapon. It’s our best defense.
- Phyllis Burgess
Lung Cancer Survivor
Tags
David Austin Gose Paulding Medical Center Daniel Leite Cardoso FortesPeopleCare Cancer Care
Related Articles

Highlights
Make Colon Health Your Habit
For many people, talking about colon health can be a little uncomfortable. However, medical issues don’t just go away if you ignore them.
Being proactive about your well-being with preventative care can help catch colorectal cancer or another serious condition early, often before it becomes a bigger problem.
Wellstar is committed to keeping your colon healthy with preventative screenings and expert care, so you can continue to live well.
Catch colon cancer early
Early detection is the best prevention, especially when it comes to colon cancer. If caught early, colorectal cancer has a survival rate of 91%.
“Colon cancer is the second most common cause of cancer death in the United States, so it’s very important that everyone gets screened,” said Wellstar Gastroenterologist Dr. Cameron Body. “For an average risk person, screenings should begin at age 45.”
Those with a higher risk or a family history of colorectal cancer may need to start screening sooner. Partner with your provider to create a personalized screening plan—and stick with it to stay ahead of the disease.
“Recently, colon cancer has been a major trending topic in public discourse, and it has been impacting younger individuals each year. It is important to start colon cancer screening at the age of 45 or sooner if you have a family history of colon cancer,” said Wellstar Gastroenterologist Dr. Shani Clay. “This is a preventable disease, so please speak with your primary care clinician or gastroenterologist to help get you screened. Colonoscopies can help prevent colon cancer, diagnose and help direct early treatment if you are diagnosed.”
The death rate for colon cancer in older adults has been decreasing for the past several decades due to screenings, according to the American Cancer Society. Screenings can identify polyps before they become cancerous and can catch cancer earlier when it is more easily treatable. However, in people under 55, death rates from colon cancer have been increasing by about 1% per year since the mid-2000s.
Why colonoscopies work
During a colonoscopy, a Wellstar gastroenterologist will view the inside of your colon and look for polyps or any other abnormal tissue that could be cancerous. This preventative testing is key to catching colorectal issues at the start.
“A colonoscopy is the gold standard when screening for colon cancer. The procedure itself is not painful, and we make sure you’re comfortable throughout the process,” Dr. Body said. “The goal is to do a high-quality exam with a good prep to find polyps when they’re small and get them removed to minimize the risk of them subsequently developing into cancer.”
Polyps take about five to 15 years to evolve into an invasive cancer, according to Dr. Carmen Klass, oncologist and hematologist with Northwest Georgia Oncology Centers, a care partner of Wellstar.
“If you have a colonoscopy every five to 10 years, they can remove the polyp and it will never be declared an invasive cancer,” Dr. Klass said. “In fact, if all Americans did their screening colonoscopies every five to 10 years, the death rate for colorectal cancer would drop by 50%.”
See how colorectal cancer screening saves lives.
Signs of colorectal cancer
- Colon cancer is typically discovered when a patient has a colonoscopy, but it’s important to watch for these warning signs:
- A change in your bowel habits, such as persistent diarrhea or constipation
- Bloody stools or rectal bleeding
- Abdominal discomfort, such as cramps, gas and pain
- Feeling like you are unable to empty your bowels completely
- Weakness or fatigue
- Unexplained weight loss
If you experience any of these symptoms, contact your care team right away.
Colorectal cancer care at Wellstar
If you have been diagnosed with colorectal cancer, count on Wellstar for comprehensive, personalized care. Our specialists will work together with you to form a tailored treatment plan and offer support every step of the way.
“When a patient is diagnosed with cancer, we walk with them and guide them on this difficult journey,” Dr. Klass said, sharing how Wellstar provides compassionate care.
Wellstar offers medical expertise close to home, clinical trials and state-of-the-art surgical procedures to treat colorectal cancer. We also have a multidisciplinary gastrointestinal (GI) tumor board that diagnoses and creates treatment plans collaboratively.
Along with cancer surgeons, medical oncologists and other experts, our care team also includes nurse navigators, dietitians, social workers, psychologists, psychiatrists and counselors to provide complete care and support.
Learn how Wellstar cares for colorectal cancer.
Get answers with genetic testing
Whether you have been diagnosed with colorectal cancer or are concerned about the chance of developing it, genetic testing can help you understand your risk of getting the disease.
If your parent, sibling or child has had colorectal cancer, you are two to three times more likely to develop the condition compared with someone with no family history. Our genetic counselors can help determine how genetic testing could benefit you and your family.
“Wellstar offers support from genetic counselors to help keep other family members safe in the future,” Dr. Klass said.
Highlights
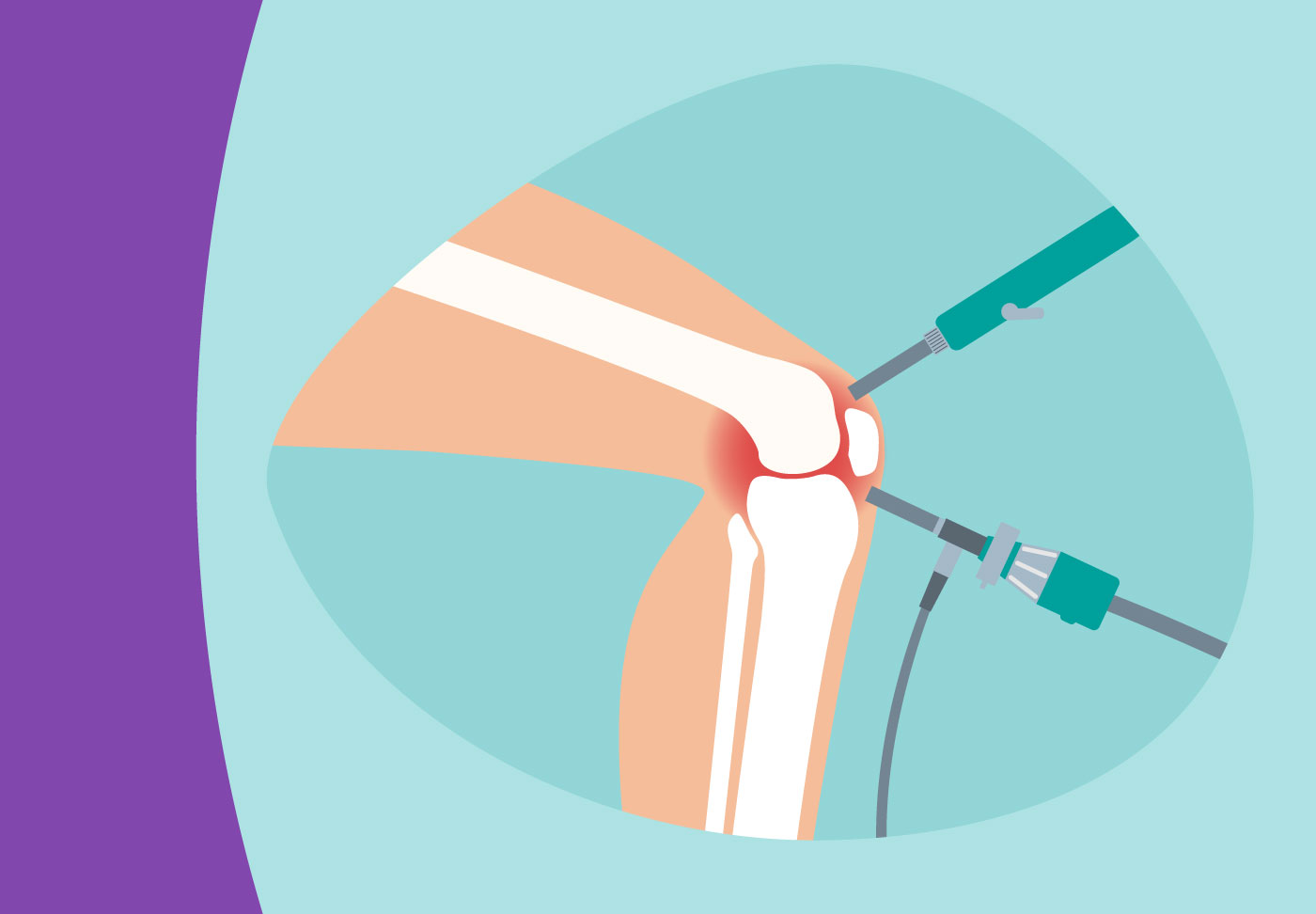
Wellstar Paulding Medical Center Offers New Smart Robotic Orthopedic Surgery
New robotic surgical technology at Wellstar Paulding Medical Center personalizes procedures and makes joint replacement surgery even more precise.
The system uses advanced imaging and data analytics, partnered with the surgeon’s expertise, to tailor care for each patient. Using a 3D model based on a CT scan of the patient’s anatomy, surgeons can plan the implant size, placement and alignment accurately before entering the operating room. During the procedure, the robotic system uses real-time feedback to guide the surgeon’s hand and touch-sensitive boundaries to protect surrounding tissues and bones.
“This robotic technology allows our surgeons to make smaller incisions, improve the implant’s placement and operate more precisely—which all mean a smoother recovery for patients,” said Todd Kennedy, president of Wellstar Paulding.
The orthopedic surgery team at Wellstar Paulding uses the system in total hip replacements and total and partial knee replacements.
Wellstar Orthopedic Surgeon Dr. Sameer Badarudeen, who has a decade of experience in robotic hip and knee replacements, was the first to use the technology at Wellstar Paulding. He said the system allows surgeons to better personalize care for each patient.
“As surgeons, we now have a much deeper understanding of optimal artificial knee placement, moving beyond the older ‘boilerplate knee’ approach that resulted in identical-looking X-rays for all patients,” Dr. Badarudeen said. “It empowers surgeons to thoroughly assess each patient's unique anatomy and then meticulously recreate the artificial knee replacement to be perfectly tailored to that individual's specific anatomy.”
Denise Fortune, whose knee was replaced using the technology, was able to go home the same day as her surgery. She had minimal pain after the procedure and now has increased mobility after several years of knee pain.
Dr. Badarudeen ensured Denise received personalized care and had the support she needed for a smooth recovery.
“I'm feeling great. I'm still going to physical therapy, and they tell me I'm ahead of where I normally would be,” Denise said.

PeopleCare
PatCare
Pat Gelisse has been dancing for 30 years. She even taught the Carolina shag for a while. It’s a partner dance, sometimes compared to Swing dancing to beach music.
But severe heart failure downgraded Pat’s dancing queen status for close to 10 years.
“I went from feeling happy to feeling like a nothing,” she remembered of that time in her life.
With a team of Wellstar heart specialists working together for her, Pat found hope and new life on the dance floor.
Heart failure masquerades as acid reflux
It started more than a decade ago when Pat lived in central Georgia. She scheduled a doctor’s appointment for what she thought was acid reflux. She popped in on a quick break from her marketing job, assuming it wouldn’t take long.
Blood work and an EKG got Pat a ticket straight to the hospital and a quadruple bypass.
“My heart got worse; it wasn’t pumping blood,” Pat said.
She was in acute heart failure, a life-threatening condition where the heart doesn’t pump well enough to deliver the necessary amount of oxygen to her body. Pat’s ejection fraction (EF)—the percentage measurement of the blood that leaves the heart each time it pumps—was only 10%. The normal range is 50 to 70%.
It was a scary time, and with a family history of heart problems, Pat was worried. She’d lost both parents to heart failure, as well as other family members.
“I just knew for sure I was going to be next,” said Pat.
Doctors from various academic institutions discussed serious treatments ranging from LVAD to transplant, but because the pumping performance of her heart improved, she was no longer a candidate for those procedures. Instead, Pat spent close to nine years managing her heart failure with a pacemaker and various medications—treatments that failed to get her back on the dance floor.
We use cookies for booking and general analytics. Learn more about or internet privacy policy.
