From catching cancer to following through with expert care, Wellstar ensures patients never have to fight lung cancer alone.
We are dedicated to early intervention in lung cancer, which improves outcomes for patients. After detection of an abnormality on a CT scan, patients are immediately surrounded by an interdisciplinary support team devoted to their well-being.
Identifying lung cancer early
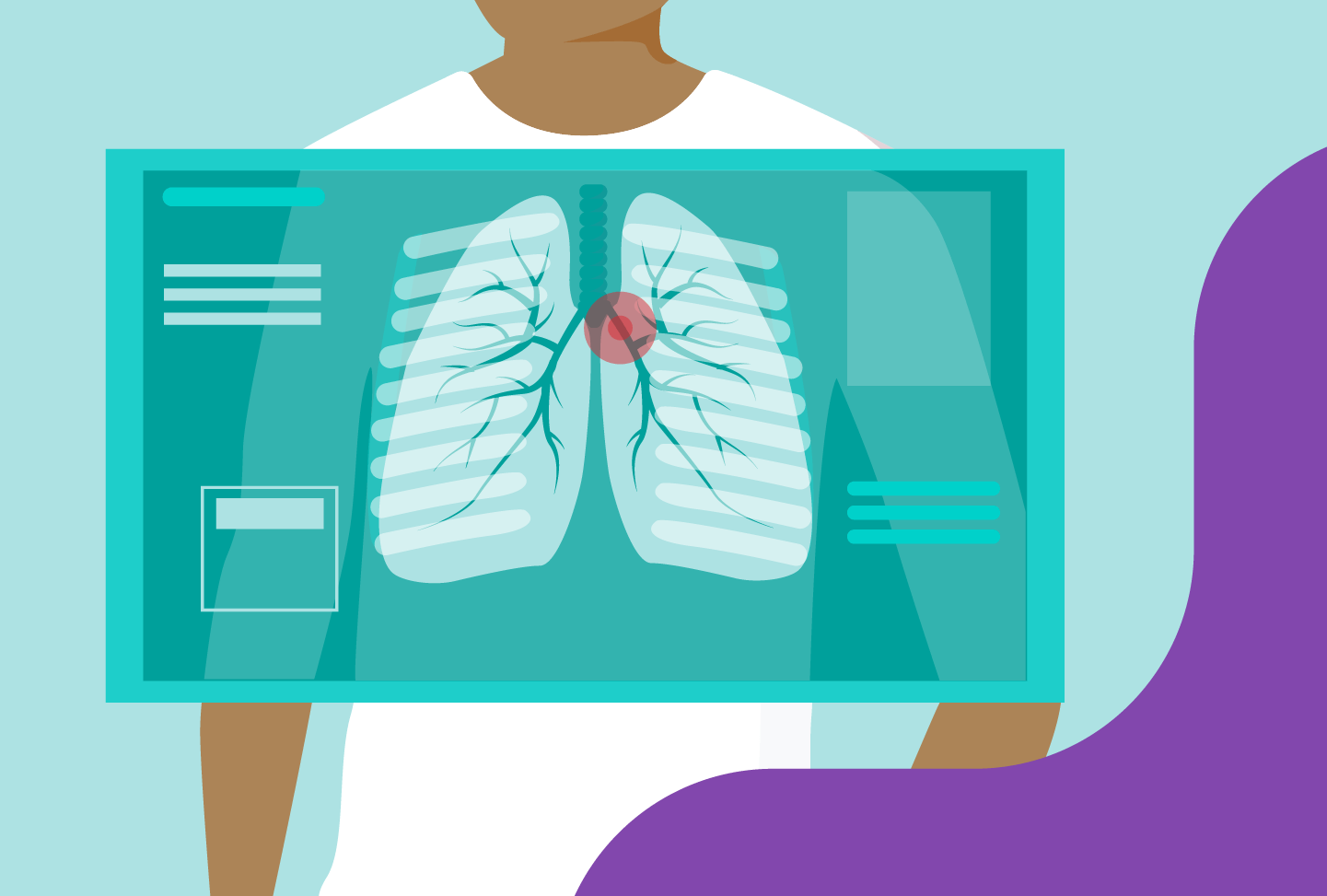
If you are at increased risk for developing lung cancer, talk to your care team about screenings. With a low-dose CT scan of the chest, it only takes a few seconds to check in on your lung health. These screenings are offered at several Wellstar imaging centers.
The United States Preventive Services Task Force has revised lung screening guidelines. Patients may qualify for screening if they are 50 to 80 years old and smoked for 20 years. If they are a former smoker, they may qualify if they quit less than 15 years ago.
“Finding lung cancer early leads to better outcomes, and screening with CT scans is recommended as the only proven way to minimize delay in diagnosis,” said Wellstar Thoracic Surgeon Dr. Daniel Fortes.
Because finding cancer and starting treatment sooner can be life-saving, Wellstar has invested in one of the nation's largest lung screening programs and an incidental nodule program. When people come into a hospital seeking care for something else—whether that be a health condition like appendicitis or a traumatic event like a motorcycle accident—they might get a scan of the abdomen or chest that also shows portions of the lungs.
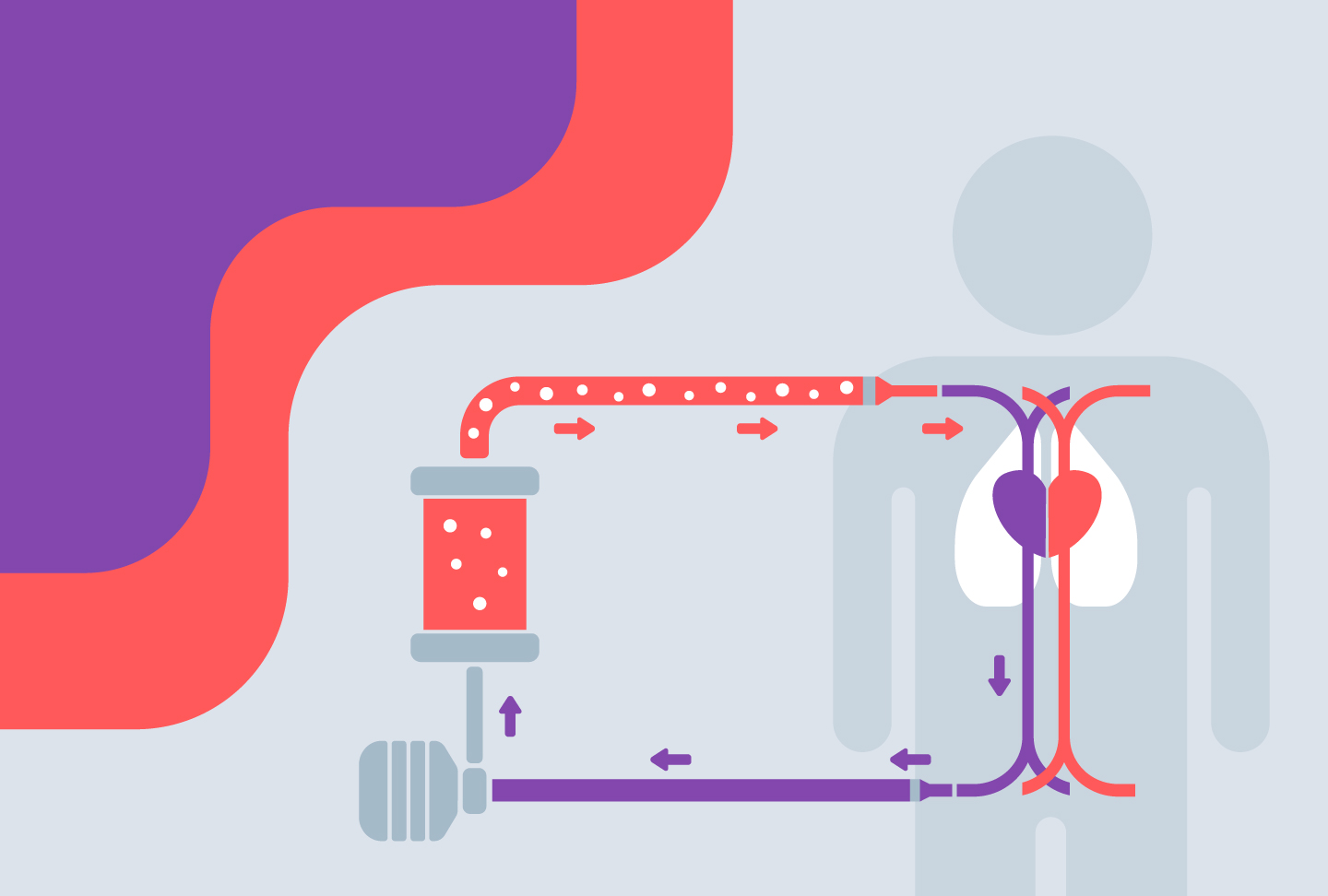
Using artificial intelligence, reports of those scans are fed to report coordinators, categorized based on their risk level and if a patient is higher-risk, forwarded to nurse navigators for review. Nurse navigators consult with physicians about the findings, and Wellstar can then initiate care if cancer is suspected.
The program, which started in fall 2020, has identified a total of 203 lung cancers and 22 other types of cancer, as of November 2025.
Expert care and support at every step
From the very beginning, people with lung cancer at Wellstar are surrounded by a team of experts. Rather than go through the time-consuming process of driving to multiple appointments with different specialists, patients meet with all these physicians in one place.
The Wellstar Lung Cancer STAT Clinic—at Wellstar Cobb, Wellstar Douglas, Wellstar Kennestone, Wellstar North Fulton, Wellstar Paulding and Wellstar West Georgia Medical Centers, as well as Wellstar Cherokee Health Park and the Thoracic NOW Clinic at Wellstar MCG Health Medical Center—give patients immediate access to specialists in medical oncology, radiation oncology, pulmonary medicine and thoracic surgery.
"We plan patients’ appointments ahead of time, ordering multiple tests that will be necessary for the treatment decision-making. These can include PET scans, CT scans, MRIs and/or a pulmonary function test," Dr. Fortes said. "We’re always gaining time in the patient’s overall treatment because we are anticipating and creating a plan as a team."
Getting multiple expert opinions from the start not only gives patients peace of mind, it speeds up treatment, too. In the United States, the average time between an abnormal scan and the beginning of treatment is 60 to 90 days. The STAT Clinic reduces that time to as little as 14 days. Time-to-treatment affects long-term survival in patients with lung cancer.
"We have data to show that if we delay treatment, even in early-stage cancers, we decrease the chance of a cure," Dr. Fortes said. "The goal of the STAT Clinic is to get them the quickest we can into their final treatment plan."
High-tech surgery options
For many patients, surgery is a crucial part of lung cancer treatment. Wellstar offers several minimally invasive options, reducing recovery time for patients.
More than 90% of lung cancer surgeries at Wellstar are performed using either the Da Vinci Surgical System or Video Assisted Thoracic Surgery techniques (VATS).
Minimally invasive surgeries reduce pain, scarring, blood loss and infection, as well as time to recover—getting patients back to work and other routines quicker.
The Da Vinci system is equipped with 3D cameras and instruments that can make very intricate, precise movements, allowing for shorter incisions and more accurate surgery. Some patients can leave the hospital as early as the next day.
For biopsies, Wellstar has completed 500 procedures using the Ion system, a robotic-assisted platform.
The system uses a three-dimensional spatial recognition technology that helps guide a catheter down the airway, deep into the lung, all the way to small nodules where biopsies can be performed. The robotic catheter maintains its shape and stability throughout the biopsy process, significantly improving diagnostic yield compared to other modalities.
"The better the image and the more certainty we have of the spatial location of the catheter, the better we can avoid complications by making sure we are not too close to a blood vessel or the edge of the lung," said Dr. Fortes.
To reduce your risk of lung cancer and keep your lungs healthy, talk to your primary care team and follow a few tips, such as exercising and avoiding smoking. Learn more about treatments on our lung cancer care page.