This article was originally published on Atlanta Business Chronicle on November 3, 2023.
As cancer research advances, doctors know more about the keys to reducing cancer cases and driving better outcomes, like long-term survival. Prevention, early detection and treatment—an area that has drastically improved through scientific discovery—are the big three keys today. While preventative measures reduce the risk, screening for cancer before someone has symptoms can be a lifesaver when it is identified earlier and in more treatable stages. Newer, more advanced treatments and starting treatment faster are also making a sizeable impact on survival. For a closer look at how healthcare experts apply these keys in the fight against cancer, Atlanta Business Chronicle’s Market President and Publisher David Rubinger sat down with Wellstar leaders and patients for a sponsored panel discussion on the state of cancer care.
Panelists & moderator
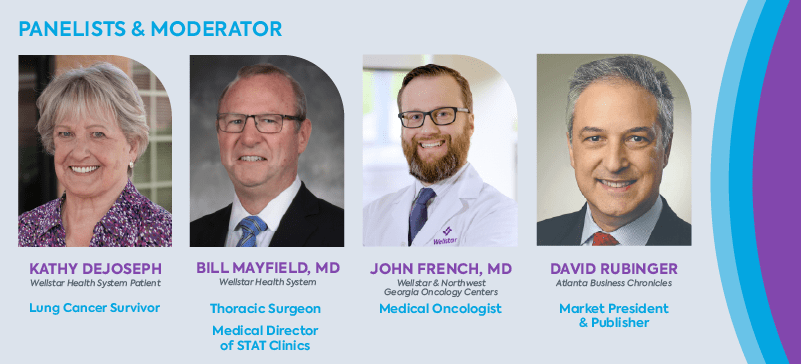
- Dr. Bill Mayfield, MD, medical director, lung screening program, medical director, incidental pulmonary nodule program, medical director, STAT Clinics, Wellstar
- Dr. John French, MD, medical oncologist, Wellstar and Northwest Georgia Oncology Centers*
- Kathy DeJoseph, lung cancer survivor
- David Rubinger, market president and publisher, Atlanta Business Chronicle
*Wellstar partners with Northwest Georgia Oncology Centers to provide world class cancer care close to home.
Keys to better outcomes
David Rubinger: Cancer is one of the top causes of death in the U.S., second only to heart disease, with 1.9 million new cancer diagnoses expected this year. The whole idea of trying to beat cancer is the common language of treatment now. We’ve really changed the conversation in many ways. Dr. Mayfield, what have been the keys to getting these better survival rates across all types of cancers?
Dr. Bill Mayfield: There are three basic components to improving outcomes and reducing cancer. Number one is prevention. How can you prevent cancer? Smoking cessation is a major way to reduce the risk for cancer, especially lung cancer. The second key is early detection screening for cancer such as colonoscopies, skin exams and low dose lung cancer CT scans.
Finally, we have treatment as the third key. We have dramatically improved treatments, especially in the last 10 years, with targeted therapies, immune therapies and precisely targeted radiation therapy. For some cancers, reducing the time it takes to start treatment can be as impactful as some of the newer cancer therapies. At Wellstar, we speed up time to treatment through our STAT Clinics.
Rubinger: Dr. French, from the medical oncology standpoint, what has specifically gone on in your world since you started practicing medicine that you think has improved these outcomes?
Dr. John French: There’s no bigger story than immunotherapy in the last 10 years. It was 2017 when Jim Allison out of the University of Texas MD Anderson Cancer Center and Tasuku Honjo in Japan won the Nobel Prize for cancer immunotherapy—the first time the Nobel in Medicine recognized a cancer therapy in decades. Wellstar and our patients participated in clinical trial development of immunotherapy for various cancers.
In medical oncology, there are also targeted therapies. In improving the survival and outcomes of patients, we do a lot of what we call next generation sequencing—tumor genomics and tumor DNA. The way I explain this is, “We’re not testing Kathy’s DNA. We’re testing the tumor itself. We are trying to find a lock and key mechanism, where if we can find what’s driving the cancer, maybe there’s a pill or a target that we can go after to take it out.”
Rubinger: Let’s move on to lung cancer in particular. Lung cancer has traditionally been known as a smoker’s disease—at least that’s how many people view it. It appears as though in the United States we’ve seen an improvement in terms of the number of lung cancer cases. Dr. Mayfield, where is the lung cancer discussion right now? I feel it was maybe one of these small victories that are going on in the cancer movement.
Dr. Mayfield: We do actually have some large victories. The surgeon general came out with a report in the 1960s that said smoking caused premature death and lung cancer. Men in Georgia started reducing their smoking about 35 years ago. As a result, we have 50% fewer male smokers and 35 years later, we’re now seeing a 50% reduction in primary lung cancers from tobacco.
Rubinger: As far as I understand it, early lung cancer is one of those cancers that has no outward physical markers that tell you you’ve got something going wrong. So as lung cancer specialists, what do you advise people to do when they’re getting their checkup? What is the process by which they should be screening for lung cancer?
Dr. French: The biggest thing you can do is if you’re smoking, stop smoking and get screened if you’re eligible. Dr. Mayfield discussed that already, but I’ll add some numbers and perspective.
Number two, if you were a smoker, understand the guidelines and recommendations to undergo screening. They updated the guidelines in 2021 that if your age is 50 to 80 and you have a 20 or more pack per year history of smoking, and currently smoke or quit within the past 15 years, then you’re eligible for screening.
By having a CT scan, you can reduce the risk of lung cancer death by up to 20% by identifying and treating cancer earlier.
Rubinger: Let’s talk to a lung cancer patient about this. Kathy, thank you for joining us. Take us briefly through your journey. What is your background with cancer?
Kathy DeJoseph: This year, I’m a 12-year survivor. Before I was diagnosed, I was a career person and I was on my computer one day and up popped information about this early lung cancer screening study that Wellstar was a part of. I had no symptoms. I had a long history of smoking, grew up with parents who smoked, grandparents who smoked, lived near a factory that was belching out junk into the air.
I was a workaholic and a mom and I saw this study and for whatever reason, I called and talked to the nurse navigator. I was like, “I don’t know whether I want to do this or not. You know, this sounds like I’m going to end up paranoid about it.” She encouraged me to participate.
Dr. Mayfield: Kathy was enrolled in the study and had three or four normal CT scans before she developed a mass. And sure enough, we jumped right on it through Lung Cancer STAT Clinic and got her treatment plan together quickly. That was the point of her being in the annual screening study.
What is a STAT Clinic?
Rubinger: Kathy, before we dive further into your treatment, will Dr. Mayfield help define the STAT Clinic? It’s not a simple thing to do. You all are very busy people and you all have individual schedules. To turn you all into this sort of troop, if you will, moving in sync, that’s a logistical nightmare for a bunch of doctors.
Dr. Mayfield: STAT stands for Specialty Teams and Treatments and it’s about bringing multiple cancer experts together to collaborate about a patient’s care and meet with them the same day so they can get treatment started quickly. We created STAT because we saw a need to do things better and to put the patient at the center of everything we do.
About 17 years ago, we opened a general Thoracic Surgery practice at Wellstar Kennestone Regional Medical Center. And we did everything like everybody else did. We had a navigator—someone who connects a person who has cancer with the help and support they need. We had tumor boards—a group of physicians and scientists who meet to discuss treatment options for individual cancer patients.
But when we looked carefully, we saw that by the time the patient’s case was presented in a tumor board, it was 58 days on average from the time the patient had their original CT scan. They had gone from a primary care doctor to a pulmonologist to an oncologist back to the pulmonologist, then had a biopsy, a PET scan and then maybe saw a radiation oncologist. It was 58 days by the time they got to the tumor board and were able to get a treatment plan started. That’s a problem. But that is the standard of care in the United States today—60 to 90 days in this workup period.
We said, “There’s got to be another way.” I knew of a clinic run by a pretty notable oncologist in another state, who brought the thoracic surgeons, pulmonologists and the oncologist to his clinic to see the patient at the same time. An oncologist and I drove up there, spent the day, asked a bunch of questions and said, “You know what, we need to do this.”
So we came back and getting those specialists—the thoracic surgeon, pulmonologist, medical oncologist, radiation oncologist and navigator—in the same place at the same time was hard.
What we decided to do is start with one hour on Wednesday afternoon. So we saw two patients one week, then 2 to 3 the next week and then 3 to 4 the next week. Then a primary care doctor heard about it and the pulmonologists heard about it and suddenly we were seeing 12, 15, 20 patients.
A few years ago we surpassed more than 10,000 patient visits in the Lung Cancer STAT Clinic. And during that time, we started the lung screening program and the incidental nodule program.
The culmination of our initiatives to identify lung cancer earlier and hasten the time to treatment has reduced our time from abnormal image to starting treatment to somewhere between 14 and 20 days, rather than 60 to 90 days. The early detection program has made it such that 40% of the cancers diagnosed at Wellstar are stage 1 and 2, when cancer is more treatable and patients have better outcomes. On a national average, just 15 to 20% of lung cancer diagnoses are stage 1 or 2. We’ve dramatically improved the ability of our lung cancer patients in our community to survive their disease.
Rubinger: It sounds like early detection and shorter time to start treatment make a real impact for patients. Kathy, let’s talk a little bit about what those things meant for you as a patient. Let’s start with when you were diagnosed. Did you have any symptoms? What happened next?
DeJoseph: I didn’t have any symptoms. Everything was fine, except for my history with smoking. The year I was diagnosed, I was going to quit the study but the nurse navigator took me out to lunch to convince me to come back—and thank goodness she did. I was diagnosed the very next day.
The biggest benefit for me with the way the STAT Clinic works is that I didn’t have to worry about whether the doctors had actually talked to each other. I didn’t have to worry about whether maybe they didn’t actually agree. All those things that I would have been worried about went away because I talked to all of them on the same day in the same place.
It gives you a lot of confidence. I thought, “Well, you know, they’d have to all be wrong on the same day at the same time to screw this up.” I ended up becoming a volunteer and would meet with newly diagnosed patients for several years. One of the biggest things that I would talk to new patients about is how STAT Clinic kept things from dragging out for months, going from doctor to doctor.
Rubinger: It sounds like STAT Clinic is meaningful to patients, not just medically, but emotionally. Is the STAT Clinic exclusively for people with lung cancer or are patients with other conditions benefitting from this model now?
Dr. Mayfield: That’s a good question. We added Lung Cancer STAT Clinics at Wellstar Cobb, Douglas and North Fulton Medical Centers. Outside of lung cancer, my neurosurgery buddy got curious. He’s saying, “Wait a minute. You know, we have this patient with brain cancer and they have to go see the radiation oncologist but your patient gets to meet the radiation oncologist at the same time as you. We want that.”
So the next STAT Clinic that cranked up was for neurological tumors. It was awesome to see that we could inspire other folks to do the same thing.
Dr. French: To add to that, we also have STAT clinics for breast cancer and head and neck cancer. All of these cancers require multidisciplinary care with doctors from different specialties who collaborate on patient care because otherwise, you have to go see different cancer subspecialists and that may take a longer period of time.
Dr. Mayfield: Here’s the dark secret about cancer care in the U.S. Dr. Alok Khorana at the Cleveland Clinic published a paper about three years ago. He studied 1.2 million cases in the national cancer database and 340,000 of those were lung cancer patients. He clearly showed that for every seven days’ delay in therapy in stage 1 or stage 2 disease, you lose 2% five-year survival. Delay in time to initial cancer treatment in the U.S. is an important risk factor for survival over time.
A first-hand account
Rubinger: Kathy, let’s come back to you for a second. So you go into this STAT Clinic. Obviously, this whole process must have been terrifying on so many different fronts.
DeJoseph: I wasn’t as terrified for as long as most people are because I had answers within a short period of time.
Rubinger: How short?
DeJoseph: I had my biopsy the next morning after the first STAT Clinic appointment. About a week and a half after that, I started chemo. That was really fast. I had surgery after chemo.
In the STAT Clinic, every doctor comes in and talks to you. You learn what their role is going to be and what the timing will be with other treatments. It all happens at the same time. I took a lot of confidence in questioning everybody on the same day and knowing they had also talked together. I knew for sure that they had, where I would have really wondered about that if had I done it the normal way—visiting multiple specialists over a several-month period.
Rubinger: I’ll be the contrarian for a second. What if I walk into the STAT Clinic and say, “Well, I’d like to choose my surgeon. I’d like to choose my oncologist. I’d like to choose the radiation oncologist I want to use for my radiation treatment.” How much flexibility do I have within the STAT Clinic to select the doctor I want to work with? Or do I have to take the ones that are assigned to me regardless?
Dr. Mayfield: That is an excellent question. You can come to us for a consolidated opinion and get your care wherever you choose. You have four experts looking at you physically and reviewing all your imaging and all your tests together, coming to a consensus. For treatment, you can use any oncologist, any thoracic surgeon, anybody you want, even if it’s within our own institution.
Dr. French: Whether we’re providing the care or simply an opinion, STAT Clinic puts the patient first. We have patients from Alabama, Tennessee, North Georgia who can’t travel here for ongoing care. I’ve even had patients who live near the Carolina border. Part of the STAT Clinic is also handling the logistics where one of these patients may need treatment closer to home. For example, someone may need chemotherapy and I say, “OK, I’ll coordinate that with the medical oncologist in your area.” When we’re done seeing STAT Clinic patients, we agree, “You call the local radiation oncologist, I’ll call the local medical oncologist and let’s get them plugged in and connected with treatment recommendations.” Again, STAT Clinic expedites and coordinates all that care. Getting the foot in the door and getting that ball rolling is half the battle.
The state of screening and future goals
Dr. French: In talking about screening earlier, we didn’t address non-smokers. If I don’t smoke, I don’t need to be screened if I’m doing my well check-up and I’m not having a cough or chest pain. There’s really no screening for lung cancer outside of those recommendations.
That being said, the other thing that you need to understand is that in the state of Georgia, we are horrible at screening people. We rank toward the bottom quartile of the entire country in screening patients when it comes to the proportion of eligible patients. The American Lung Association data ranks Georgia 35th in the nation. We screen 5% of eligible people, so we’re not capturing 95% of people who could be screened.
We know the data to support screening is there. Kathy is a living example of this. Talk to your primary care doctor about your history with smoking and the need for screening.
Dr. Mayfield has ramped up the effort to capture more at-risk people through screening, but we still need to get the message out.
Dr. Mayfield: We started our screening program 15 years ago as part of I-ELCAP—the International Early Lung Cancer Action Project—and then we broke off of the study because the results were so positive. We decided we’re just going to do this as a standalone program in our community.
As a result, over the last 15 years, we become one of the three largest lung cancer screening programs in the U.S. We have about 15,000 people in our program currently.
The problem is, we serve a community of 1.7 million in 15 counties. Knowing that 40% of those are smokers or former smokers, we should be scanning a million people a year.
Why aren’t we screening more people? We’re a part of the Georgia Lung Cancer Roundtable and the National Lung Cancer Roundtable trying to solve that problem. I think it’s going to take a national awareness campaign.
When that happens, we need to prepare our screening centers for high volumes. That will drive us from discovering more stage 3 and 4 lung cancers when people are dying, to finding more stage 1 and 2 lung cancers. Those earlier-stage cancers are much less expensive to treat from a policy and population health level and are easier to treat, giving more patients good long-term outcomes.
Rubinger: But we wouldn’t be screening non-smokers at this point.
Dr. Mayfield: There’s not enough data yet to guide us to any other risk factor than tobacco use.
What employers should know about cancer
Rubinger: Let’s talk about the business community for a second.
When it comes to the employee, when you see patients who are in full-time jobs, what role do you see the employer playing when you’re caring for cancer patients? What can employers do to help them in their battles?
Dr. Mayfield: I have a pretty strong opinion on two items. One is that employers should promote age-appropriate screenings for all cancers among their employees. Give them that half a day off if they need to go somewhere for a doctor’s appointment to get that screening exam. And as callous as it may seem, that half a day off to find cancer in earlier stages is much less expensive than treating an advanced cancer years later, from extended time off to the insurance costs associated with advanced cancer.
The CEO of the corporation, the vice president, the chief medical officer, the chief operating officer—they assume that if they or any of their employees get cancer care, they’re going to get the best care available. But unfortunately, the best care available today in most places is going to take them 60 to 90 days to get through the initial doctors’ visits and tests that at the STAT Clinic, we manage in 14 days.
My challenge to the business community is to ask their insurers and their healthcare providers a very difficult question, “How long will it take to get our employee from an abnormal finding to starting treatment?” When insurers and healthcare providers have to start answering hard questions, then we’ll move the ball.
Dr. French: I would add, when a corporation buys health insurance, it needs to make sure institutions that perform research and clinical trials are covered.
I had a patient who had stage 4 prostate cancer and there is a clinical trial using novel bispecific immunotherapeutics. The guy is young; he’s eligible for the trial. The patient signed the trial consent only to find out that his insurance doesn’t cover the medical facility that’s offering it, so therefore he’s not eligible for the clinical trial. Now he’s going to have to get the standard of care, which is good. But he could have gotten something new on a trial if it was covered by his company’s health plan.
So, companies should first make sure that employees are covered for good quality healthcare and at top facilities that perform research.
Number two is, if you’re an executive, consider supporting on-site screening. I’ve seen a lot of patients in the STAT Clinic who get executive physicals, they get a day off and they do this comprehensive testing. Lo and behold it shows something. That early detection gets them to treatment at an earlier stage when the cancer is less advanced and they have a higher chance for better outcomes.
So consider offering a half-day, a health fair or on-site health screenings as part of your company’s health offerings.
I think a healthy employee, one that feels valued and respected, will be a hard worker. If I feel that my business cares about me, my health, my life and my family, that sounds like a company I’d want to work for.
Learn more about cancer care at Wellstar.