This article was originally published on Atlanta Business Chronicle on February 9, 2023.
Cardiovascular disease is the leading cause of death in the United States, claiming more lives than all forms of cancer combined. Heart disease and stroke are among the forms of cardiovascular disease. In 2019, nearly 900,000 people died of cardiovascular disease in the United States, according to the American Heart Association. In Georgia, about 1 in 3 deaths are caused by cardiovascular disease, according to the Georgia Department of Public Health. Most of these deaths are premature and preventable. Atlanta Business Chronicle recently talked with a panel of experts from Wellstar Health System and the American Heart Association about ways to accelerate heart care progress through diversity and inclusion and finding better ways to fight heart disease through unconventional methods, early detection and education and through the workplace.
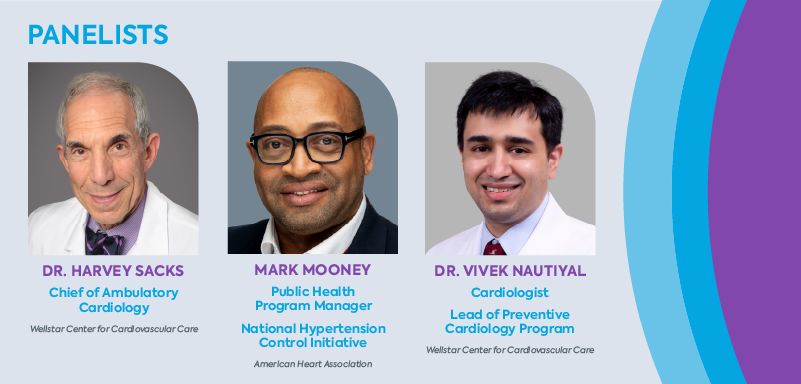
Panelists & moderator
Moderator: David Rubinger, Market President & Publisher, Atlanta Business Chronicle
Rubinger: What is the best way to define heart disease? And what does it mean for our culture?
Dr. Vivek Nautiyal: Let me start by saying that heart disease or cardiovascular disease is a very broad term which include a wide variety of conditions affecting our heart and blood vessels. The most common type is coronary artery disease, which is usually caused by cholesterol plaque clogging the arteries, supplying blood to our heart. This is the number one cause of death in the U.S. and across the world.
Some other types of heart disease include heart failure, which affects the heart muscle pump, heart valve disease and heart rhythm disorders affecting electrical activity of the heart. Vascular disease includes aortic aneurysm, and disease affecting neck arteries going to the brain or arteries going to the legs. All of these would broadly come under heart disease.
These conditions affect the ability of the heart to function properly and can lead to serious health problems such as heart attacks or stroke.
Rubinger: How much of that would we consider to be genetics and how much would we consider to be lifestyle, leading to the disease itself?
Nautiyal: Genetics is important, but I would say the vast majority are lifestyle-related. And that is why it's killing so many people. Heart disease is often the result of lifestyle factors like poor diet, lack of exercise, mental stress.
About 4 in 10 U.S. adults currently are obese; 3 in 10 have high cholesterol; 4 in 10 have hypertension; 1 in 10 have diabetes. So, this is an epidemic. Adolescent and childhood obesity is on the rise and we in Georgia are sitting in the diabetes belt of the U.S.
Lack of awareness of these common risk factors often leads to delay in seeking preventive or medical care. You can have hypertension, high cholesterol, and diabetes for years or decades without knowing, which is why they're called silent killers. Unless you check for them, you may be blissfully unaware of your risk, until one day it leads to a major event.
Rubinger: It's very common to hear about examples where sometimes it can be genetic and other times it can be a lifestyle cause. Dr. Sacks, in your career, how have you viewed this whole conundrum of how to best approach heart disease?
Dr. Harvey Sacks: Getting back to your previous question, one form of heart disease we did not mention is congenital heart disease—malformations of the heart and blood vessels which occur at birth. As regards to lifestyle, when I started practicing cardiology, I saw patients in Paulding County. At that time, it was a rural community, but it is not so rural anymore but rather an extension of Atlanta. Many members of that community had a lifestyle consisting of poor dietary habits, lack of exercise, cigarette smoking and use of smokeless tobacco.
We began an educational process to teach people about healthy living. We socialized this into the community by giving talks to schools, churches and Rotary Club meetings.
The community bought into these new concepts, and we have made great progress. We have made significant changes as a result of this education in heart attack rates and cardiac mortality in that community.
Rubinger: Do we have any data to support that?
Sacks: We do. Since we have been seeing patients in Paulding County, data show a decrease in cardiac mortality. People understand the risk factors that contribute to the development of heart disease. And this trend is not unique to Paulding County. Similar efforts have been successful throughout the country. The American Heart Association (AHA) has helped us educate millions of people, and as a result, people are adopting healthier choices.
Unconventional weapons: Collaboration, technology & more
Rubinger: From a medical standpoint, what have you learned from research that has helped deliver better outcomes?
Nautiyal: As Dr. Sacks was mentioning, we have made huge advancements in improving cardiovasular mortality and morbidity, especially in the Medicare population. There's clear evidence of that in the last two decades. One area where we are lagging behind is in the young population. Unlike the older population, in the younger population the event rates are either flat or going up.
One of the reasons for this is that traditional risk factor calculators tend to underestimate cardiovascular risk in young people. By young people, I mean below 50. So, if you are below 50 and you have family members who had premature events or if you have very high cholesterol, or if you are a woman with certain complications during pregnancy, then be aware that traditional risk factors will underestimate your cardiac risk. Also, younger people tend to have this sense of invincibility. You don't have any symptoms. You think, “I’m doing OK,” not realizing that silently, processes are going on in your body which one day will lead to a catastrophic event.
As part of an NIH-funded four-year study, led by the Mayo Clinic, we at Wellstar are implementing a shared decision-making electronic tool called CV Prevent Choice in our primary care offices. This enables the patient and physician to have a discussion about their personal risk for heart attack over next 10 years. It shows in an easy-to-understand graphic the impact of lifestyle measures, like healthy diet and exercise and—if needed—medications, in reducing their cardiac risk. We collaborated with the Mayo team to include factors on this risk calculator, like family history, women-specific risk factors and coronary calcium score, which alerts the clinician and patient that actual risk may be higher than indicated.
Another area where we in the U.S. lag behind is utilization and adherence to easily available life-saving therapies. A recent study showed that in over 600,000 commercially insured patients with established cardiovascular disease in the U.S., the utilization of appropriate, life-saving medications, such as statins, was low, despite overwhelming evidence of the benefit and established clinical guidelines. Only 1 in 5 patients received appropriate high-strength statins, despite these being relatively inexpensive generic medicines. Younger patients and female patients were less likely to receive these therapies. Furthermore, patient adherence, as measured by prescription refill rates, was low.
To better understand some of the factors behind this and also improve our quality of care, we at the Wellstar Center for Cardiovascular Care are honored to have been chosen by the American Heart Association, to be 1 of 6 healthcare organizations across the country to participate in an integrated cardiovascular cholesterol management initiative, a learning collaborative grant. As part of this initiative, we will track patients admitted with heart attacks and follow them as they transition home. We will pilot programs to get patients to their treatment goals within a short time after discharge and improve patient outcomes.
Rubinger: Mr. Mooney, why aren’t people taking their statins? Is this part of the problem? Are people making bad decisions based on lack of education about what the risk factors are?
Mooney: There are a lot of factors that play into why patients are not adhering to taking statins or medications. Some of those barriers are health literacy, access to healthcare, and the affordability of medications. The expansion of Medicaid could address some of these factors. We at the American Heart Association are supporting the states that are advocating for Medicaid expansion.
Rubinger: What have been the major technological changes that have really made your jobs more effective or easier?
Sacks: There are different kinds of technology. One type is the evolution of the treatment of coronary heart disease. We are not only able to diagnose blockages in coronary arteries, but in a large proportion of the patients we can treat them with stents, reserving surgery for more extensive and complex heart disease. We are treating patients with valve abnormalities without having to open their chests, thus providing a much less invasive procedure.
A spot on the lung, or pulmonary nodule, is sometimes found incidentally on a CT which was ordered for another reason. We have an AI (artificial intelligence) program to follow and surveil these nodules for the possible development of lung cancer. And in addition, some of these patients have been found to have enlargement of their aorta (known as an aortic aneurysm). AI can identify these patients from a narrative report. They can then be referred to medical and surgical specialists for treatment. This helps prevent an otherwise fatal event from rupture of the aneurysm.
The other part is virtual visits. We believe that virtual visits are the future. There are so many people who for many, many reasons cannot come in to see the doctor, whether it's a transportation issue, whether it's having childcare, finances, whatever it may be. We want to bring those technologies to the person when they can't come to us. We believe that we can really influence people's lives greatly by being able to do that technologically by virtual visits.
Rubinger: And virtual medicine was something really born out of the pandemic. Is the concept of virtual medicine here to stay, Dr. Nautiyal?
Nautiyal: I believe so. The idea was there before, but the pandemic forced us into implementing it a very short time span. Now I think it's going to stay, but in a hybrid model. In-person conversation and physical exams still have meaning in spite of all the technology. An example of a hybrid model would be if someone was hospitalized recently for heart failure and now needs frequent visits for adjusting medications, they don't have to come in every time. We can do virtual visits to adjust the medications and get them to their goal.
Sacks: Psychological ill health can be as important as physical disease. Wellstar has introduced a Cardiovascular Behavioral Health program which can in part be virtual. It integrates behavioral health with physical wellbeing. We can help patients identify emotional problems which can contribute to physical maladies. Obesity is a prime example.
Obesity is often stigmatized, but it is actually a disease. And when you recognize it as a disease, you can treat it as such, similar to how we can treat other conditions. We can do a lot of this support virtually. We also have medications to curb obesity and even surgery for complex cases. If we eliminate the stigma associated with certain conditions, we can better treat them. We need to recognize emotional triggers which can lead to physical medical issues.
Prioritizing early detection
Rubinger: You mentioned earlier younger people who may think they’re invincible. These are the people who need to learn about early detection, earlier on in their lives. What is the recommendation you all give to the younger population to start monitoring their own heart health to know whether they need help? What are the steps younger people need to take to make sure they are addressing these issues?
Nautiyal: I would like to highlight two key groups who are at a very high personal risk of heart attacks or strokes. One is familial hypercholesterolemia. This is a genetic condition where you have high cholesterol levels since early childhood. The way to identify this is to know your cholesterol numbers and know your family history. Familial hypercholesterolemia, FH for short, is not as uncommon as we thought. One in 250 people have FH, and only about 20% of people with FH have been identified or recognized. This leaves a vast reservoir of undiagnosed and undertreated people. If you are a man with untreated FH, there is a 50% chance of having a heart attack by age 50, that is basically a coin flip. Women with untreated FH have a one in three chance of having a heart attack by age 60.
The second group is people with family history of premature heart attacks or strokes.
If you are in one of these two groups, I would strongly urge you to seek preventive cardiology consultation.
Regardless of whether or not you belong to one of these two groups, I cannot emphasize enough the importance of following a heart healthy dietary pattern, exercising regularly, not smoking, getting adequate sleep and knowing your numbers—blood pressure, cholesterol and sugar levels.
On a positive note: know that your DNA is not your destiny. If you treat FH adequately early on in life, you can have a healthy and long life without any cardiac problems. Similarly, and this has been well studied, even among people who have a cluster of genetic mutations predisposing them to heart attacks (high polygenic score), following a heart-healthy lifestyle can reduce their risk by 50%. Again, your DNA is not your destiny.
At Wellstar, we also offer a robust 'Know Your Heart' screening program for the general public to schedule an appointment. The advanced version of this includes a CT coronary calcium score. For specialized care, we have a Preventive Cardiology office, where we offer evidence-based, patient and family-centered care with a multidisciplinary team including a cardiologist, dietician, clinical pharmacist and geneticist. Our cardio-genetics program has the highest volume of patients in Georgia.
Mooney: Through programs like Kids Heart Challenge at the American Heart Association, which partners with schools to help prepare children for success by empowering them to embrace a healthy lifestyle—eat well, move more and stay tobacco free. The Kids Heart Challenge prepares elementary students for future success both physically and emotionally. Through cardio-pumping physical activities, kids learn the importance of being heart-healthy. Participating schools and/or teachers receive discounted certificates for PE equipment, direct contributions to their school and new curriculum resources for whole-child centered learning. Healthy students are better learners; teachers and schools have a major influence on students’ health, and the Kids Heart Challenge is designed to support and improve those efforts.
One other AHA program, Target BP (blood pressure), using the M.A.P. (measure accurately; act rapidly; partner with patients, communities) Framework is connecting the community to clinics. This program here at the American Heart Association is designed to work with clinicians with improving how blood pressure is measured, developing treatment algorithms to improve uncontrolled blood pressure. This program’s framework was used to train barbers and stylists in an initiative called “Do You Know Your Numbers?”
We worked in barber shops and salons, faith-based and community-based organizations to install blood-pressure monitors and train them on how to use them. In the barbershop we talk about sports, families, children, so within that conversation it was simple to bring up “do you know your numbers?” And once they asked that question, and their clients are interested in knowing their numbers, they are able to screen those clients for high blood pressure. The people who need medical care are connected with health centers or clinics.
It has worked and it has grown and it's nationwide. We sent this national hypertension project throughout so many different communities, whether rural or urban. We find that bringing in that community component helps get patients to seeing their clinicians.
Education to reduce the numbers
Rubinger: Education about cardiovascular disease risk factors clearly plays a big part in helping people avoid making bad decisions. What programs or initiatives have had the biggest impact?
Sacks: If there is a group of people that we have significantly impacted, it is women. Mr. Mooney can speak to this too. You know, if you ask a woman what is she most likely to die from, she will probably tell you breast cancer or uterine cancer. But the truth is she is most likely to die from heart disease. The AHA has highlighted this with their Wear Red Day events and other programs. Women have come to understand their cardiac risk, and that their symptoms of heart disease may differ from those of men.
Mooney: I would agree with you on that. The information, as it relates to women dying of heart disease, is really the approach of addressing social determinants of health.
And quality improvements are really about self-management. For example, with the blood pressure project, it is a way of educating the patients, empowering the patients to take control of their blood pressure through what the doctors have shared with them. Talking to and educating these patients, as in the example Dr. Sacks gave in Paulding County, helps them know what are those factors that impact their health, such as healthy eating, access to care, also access to medication.
We're discovering in this hypertension research project that these populations would not have had access to blood pressure monitors outside of the doctor's office to get true blood pressure readings. That's self-measurement. Now these devices, when they check their blood pressure, it automatically links up into their EMR systems. It's all about time: the patient comes from that (screening) to a follow-up appointment. Doctors have a real clear big picture of what the patient’s true blood pressure readings are, and that's where it goes into better treatment plans as it relates to physical activity, diet, and so forth.
Sacks: That recent study involving stationing pharmacists in predominantly African-American owned barber shops demonstrated the power of education. They screened patrons’ blood pressure. A large number of men, with no prior medical history, were found to have significant hypertension (high blood pressure). These individuals were then placed on medication. It was an amazing study because they were able to identify, educate and treat these patients thus reducing their risk of heart attack and stroke.
Rubinger: The key here is my numbers. My primary care physician needs be looking at those numbers closely, even though I am a younger person, because they're the bridge to getting referred to take care of these conditions. Is the primary care system addressing the hard health issues in cardiac care?
Nautiyal: When we started the Preventive Cardiology Program about two years ago, we took a holistic or multi-pronged approach for this very reason. When thinking of cardiovascular risk in the population, you can imagine a pyramid. At the base of the pyramid are people with traditional risk factors like obesity, high blood pressure, high cholesterol. As you move up this pyramid, you will have more serious risk factors—for example, diabetes—and at the tip of the pyramid would be people with familial hypercholesterolemia or family history for premature heart disease, who are fewer in comparison to the base, but have highest personal risk.
We'll make the most impact by focusing on the base, because that's where the most patients are and that can be addressed adequately at the primary care level or through community-led initiatives.
And we at the Wellstar Preventive Cardiology Program are engaging with our primary care colleagues to accomplish this through the initiatives I mentioned earlier, helping them in their own preventive strategies and identifying those at the tip of the pyramid, with higher personal risk who will benefit from specialized preventive cardiology care.
Mooney: That's what the American Heart Association is all about: bringing awareness on heart disease to rural and urban communities and vulnerable populations. We are developing science based tools and resources for clinicians and providers to keep them informed with the current research and what's going on out there, as well as providing educational tools in all languages for their patient population.
We discovered that patients heard the numbers but didn't know what they meant and didn't know how they impacted their bodies. We design educational materials for these patients to really understand the consequences of high blood pressure for any literacy level. For example, in some workshops with patients and the community, we may use infographics of a home water hose connected to a street fire hydrant as an example of blood vessels to the heart and/or a boxer beating the kidney to give a visual of what high blood pressure does to the body organs. Blood pressure has impacts on your entire body. Giving the visual, just keeping it simple and straight to the point.
Rubinger: It's all about trust, right? They have to trust the medical system. There are certain communities that in the past have not trusted the medical establishment.
Mooney: Absolutely. That's why we are such a big proponent of diversity in the workplace and bringing young scholars, HBCU scholars, historical black institutions and biomedical students into this arena, connecting them with cardiologists and scientists throughout their undergrad, up into medical school and up into their careers. That's key. And that's important because getting out there in the community is key to building that trust. People trust people who are very familiar with their environment.
Expanding heart care to diverse groups
Rubinger: That need to build trust between the medical profession and certain communities leads me to another issue: the disparity in different groups when it comes to obtaining medical care. How can our cardiac experts help close the gap in this area?
Mooney: The AHA has put a lot of money and research and grants focused on science-based solutions to address health inequalities through, for example, our Health Equity Research Network on Prevention of Hypertension.
I'm research-focused on cardio and oncology working in underserved communities and bringing forward awareness of the connection of heart disease and cancer, as well as putting our money back into the community to support community-based organizations that are addressing social determinants of health that could assist with improving overall cardiovascular health as it relates to addressing food insecurity, vaping advocacy work that we do in school systems throughout the country and also where we are invested into people. We're working with our historically black colleges and universities, identifying those underrepresented in the medical field and enlightening them to also become representatives in the medical field to help improve overall health and communities throughout the nation. We've been committed to that, and we're very much committed to that.
As it relates to the training for our providers and clinicians through quality improvement programs such as “Get Down With Your Blood Pressure” and our cholesterol control program as well, we are providing the research and the educational tools for providers and for patients to assist health systems. We'll start on improving blood pressure with other health systems throughout the United States and particularly in the metro Atlanta area.
Sacks: If we needed a reminder about health equity, certainly the pandemic provided us with that experience. The mortality from COVID was much higher in the African-American and Latino communities. There is a saying that a parent is only as happy as their least happy child. Similarly, the medical community should only be satisfied if everyone has access to healthcare.
We must do a lot more than we are doing to ensure a better distribution of our resources. That is our obligation as healthcare providers. We need to deliver healthcare to those who are unable to come to us, but who nonetheless are in need of our services. We need to go to them.
Winning in the workplace
Rubinger: How important is the employer towards helping deliver on some of these messages to their employees?
Sacks: From the business standpoint, employers need to offer more health and wellness opportunities for their employees. And why is that? Because if they do, their workers will spend more time at work and less time at home, sick. They will spend less time in the emergency room because of adopting a healthier lifestyle and medical conditions will be identified sooner. The more businesses can promote these kinds of internal programs, the more an employee realizes 'my employer really cares about me; they really want me to be healthy.' It's a win-win for everyone, so those programs need to be much more widespread and offered to more people.
Mooney: The American Heart Association has workplace programs where we work with employers throughout the nation and throughout Georgia. Also we work with organizations just in in terms of broadening or expanding the pool of applicants, or those in leadership, to be able to be a representation of the community in which they serve.