This article was originally published on Atlanta Business Chronicle on April 12, 2024.
Orthopedic care has evolved from injury treatment and corrective surgery into a critical component of modern healthcare. As primary care remains foundational in managing overall health, the demand for orthopedic services has surged, reflecting changing lifestyles, demographics and expectations. In any given year, 12% to 14% of the adult population will visit their physician for back pain, according to the United States Bone and Joint Initiative (USBJI).
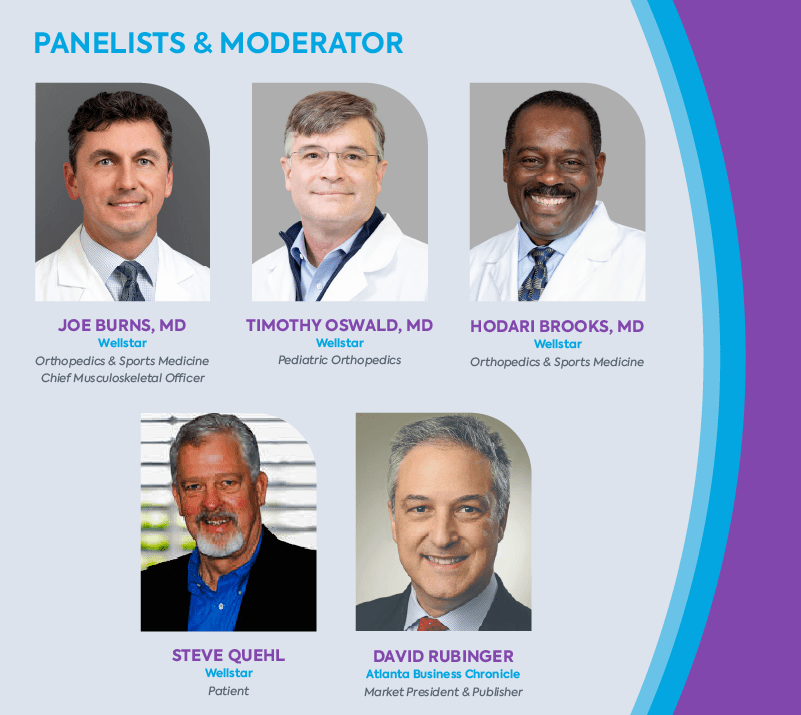
Against this backdrop of widespread musculoskeletal issues, Wellstar recently convened with the Atlanta Business Chronicle for a panel discussion to delve into the changing landscape of orthopedic care. This insightful forum explored key trends, challenges and innovations shaping the field, with leading healthcare professionals offering valuable perspectives. These discussions unraveled the complexities of orthopedic care, ranging from preventive strategies to cutting-edge treatments. Among the panelists was Steve Quehl, a former college football player for Notre Dame, who started as a tight end before transitioning to a center. Other panelists were Dr. Hodari Brooks, orthopedic surgeon, Wellstar Health System; Dr. Joseph Burns, chief musculoskeletal officer, Wellstar Health System; Dr. Timothy Oswald, pediatric orthopedic surgeon, Wellstar Pediatric Orthopedics. Moderator was David Rubinger, market president and publisher, Atlanta Business Chronicle.
The rise of orthopedics and interventions
David Rubinger: There’s an uptick in the demand for orthopedic services and these specialists have become increasingly essential to healthcare. What societal changes drive this heightened need for specialized ortho care?
Dr. Joseph Burns: We’re facing an aging population alongside a growing desire for an active, pain-free lifestyle. In the past, individuals had to endure their limitations and pain for life. Today, people have more options. Technology, techniques and training advancements now provide surgical alternatives that significantly enhance quality of life well beyond middle age.
Wellstar conducts numerous community campaigns through various channels, including community events, the media and in our offices and hospitals, highlighting the value of maintaining health and establishing a relationship with a primary care physician.
Dr. Hodari Brooks: Societal changes for both our youth as well as adults have resulted in the increased need for orthopedic care. Physical activity has decreased, with fewer kids participating in physical education. This leads to more injuries related to obesity and lack of activity. The need for joint replacements is soaring, driven by both baby boomers aging and younger individuals seeking treatment earlier. Half of my practice is caring for patients under 55, a shift from when people would wait years for treatment. Now, we prioritize improving quality of life sooner rather than later.
Patients, including those seeking joint replacements, are opting for earlier interventions. They are less inclined to wait for treatment, indicating a shift within the healthcare system towards promptly addressing patient needs.
Rubinger: What new injury trends are emerging in sports due to changing physical activity patterns, especially with the rise of extreme sports and diverse workout routines?
Dr. Burns: The rise in overuse injuries among our younger population is disheartening. Young athletes don’t diversify their sports as they once did, leading to year-round specialization and an increased risk of injury. This relentless pursuit of success often comes at the cost of rest and diversity in physical activities.
We’re also encountering complex medical issues that require specialized treatment, reflecting both advancements in medical care and the aging population’s evolving healthcare needs. Conditions once considered untreatable are now within our reach, marking a significant shift in the scope of orthopedic care over the years.
Rubinger: Dr. Oswald, as a pediatric orthopedic specialist, have you frequently observed the concept of subspecialization and the decline in diversification among young athletes?
Dr. Timothy Oswald: It’s a significant area of concern for us, and we’re conducting more research. Recent studies have highlighted the insufficient breaks and rest periods given to children, as well as the trend of starting high-level athletics too young, which aligns with the issue of subspecialization. Kids are not miniature adults. Their orthopedic stresses differ due to growth plates and differing stress responses.
We’re educating the community, including coaches and parents, about the importance of rest periods during training through channels like social media. We aim to implement better training methods so young athletes can continue playing into their college years, as we’re noticing a concerning trend where many high-level athletes quit sports as early as eighth grade.
Rubinger: Steve, as a former college athlete yourself, what’s your observation of the sports world’s changes regarding how injuries are approached, especially compared to when we were younger?
Steve Quehl: I view this issue through the lens of my grandchildren and their friends, and I agree with the insights shared by these doctors. Their perspectives must influence parents’ decisions, particularly regarding the early specialization trend. Parents often have unrealistic expectations of their children becoming professional athletes, which can lead to overtraining and injuries. Kids should have a balanced approach to sports. I’m grateful my daughters chose activities like swimming over contact sports for their children, considering the risks to growing bones and muscles.
Prior to my enrollment at Notre Dame, I appreciated the joy of playing multiple sports during each season for fun, without the pressure of turning it into a professional pursuit.
Efficient outpatient care benefits
Rubinger: I’ve noticed remarkable changes in my lifetime regarding the duration of procedures and the efficiency of hospital stays or visits to outpatient surgery centers. I’m curious about your perspective on this shift away from extended hospital stays. Do you believe it’s ultimately beneficial or detrimental to patients? What are your thoughts on this evolution of the time spent in hospitals or surgery centers?
Dr. Brooks: There’s been a significant shift in the duration of hospital stays, especially concerning joint procedures. In the past, patients would typically spend several days in the hospital before and after surgery. In my practice, around 90% of primary joint patients can return home the same day, which is remarkable. This change is not only due to patient preferences for quicker recovery but also has medical benefits, such as reducing the risk of infection. Outpatient joint replacement is not done everywhere, however, and it is important to discuss this option with your individual surgeon.
Insurance companies have started incentivizing shorter hospital stays. While this trend has clear advantages, it also comes with challenges, such as pressure to discharge patients quickly. The ability to expedite recovery and minimize specific complications is a positive development I believe will continue.
Rubinger: Do we have data showing a decrease in complications due to the trend of shorter hospital stays, particularly for joint procedures?
Dr. Burns: Evidence indicates improved outcomes for outpatient procedures, with data supporting this trend. The shift involves a comprehensive approach beyond simply performing the surgery and discharging the patient. It requires a multidisciplinary effort, with investments in establishing preoperative optimization programs, patient education classes and a coordinated team approach on the day of surgery.
Patients undergo physical therapy before returning home, but the care doesn’t stop there. We must ensure effective pain management, minimize infection risks and create a safe home environment to support their recovery. This process goes beyond safely discharging patients. It’s about ensuring their complete and safe recovery. I’m proud of the extensive teamwork and complex processes that Wellstar has implemented to support these programs.
Quehl: When it was time to correct my right shoulder this past year, I went in the morning and came back home in the evening. Dr. Burns assured me that I’d be home the same day, and it was a wonderful experience. I didn’t want any overnight stays. It was well-planned and executed, with proper anticipation and expectations set. The follow-up was excellent, too.
Dr. Brooks: Patients are shocked or hesitant when I inform them that they’ll go home the same day. It’s about managing expectations and explaining the benefits, especially as it relates to improved outcomes. Involvement in these programs gives physicians more control over the process. It’s a serious undertaking but rewarding because we can provide more input, especially in an outpatient setting. Collaboration with anesthesia colleagues has improved, particularly with techniques like regional blocks, as patients need to be up and about after surgery. Almost universally in my experience, patients prefer their outpatient surgical experience to any previous hospital stays.
Multimodal pain management success
Rubinger: This leads me to my next question regarding opioids and pharmacology. Has pharmacology evolved over the last decade to improve patient treatment?
Dr. Burns: Most of us are employing what we refer to as multimodal pain control, which involves a process aimed at sparing, if not entirely eliminating, the need for opioids as a primary method of pain management. By utilizing different medications that target distinct pain receptors, we can effectively manage pain while minimizing potential side effects that may arise from relying solely on opioids or multiple doses of the same medication. Advancements in regional blocks, administered by anesthesiologists, allow injections that can provide numbing effects in the affected areas for several days, alleviating initial post-operative pain and reducing patients’ overall need for pain medication over time.
Dr. Oswald: The opioid crisis in the greater Atlanta area is a significant concern for both children and adults, and it’s something we’re all acutely aware of. We’ve initiated extensive research efforts at Wellstar to address this issue and lead advancements in pain management that don’t rely on narcotics. Similar to the approach described in the total joint experience, we’ve been observing this trend for some time now, even in pediatric cases.
When I trained for pediatric spine surgery 20 years ago, patients stayed in the hospital for at least a week post-surgery. By implementing multimodal approaches, we’ve managed to reduce narcotic use by nearly 90% while also transitioning from a week-long hospital stay to just a 23-hour observation period for certain procedures.
Patient satisfaction is higher with these approaches, directly correlating with their overall experience. Are we expediting discharge solely for the sake of pushing people out? Actually, no. It’s about ensuring patients feel empowered in their recovery process, with their pain managed effectively, and their ability to return to the quality of life they desire. These patient-centered care programs optimize outcomes and enhance the overall healthcare experience.