Joseph Burns, MD
Specialties
Orthopedic Surgery
Education & Training
Doctor of Medicine
Joseph Burns, MD
Orthopedic Surgeon with Wellstar since 2020.
Specialties
Orthopedic Surgery
Education & Training
Doctor of Medicine
Office Locations
Expertise
About Joseph Burns, MD
Joseph Burns, MD is the Chief Musculoskeletal Officer at Wellstar, overseeing orthopedic surgery, pediatric orthopedic surgery, sports medicine, orthopedic trauma, hand surgery and podiatry. In addition, he is a practicing, fellowship-trained orthopedic surgeon who specializes in shoulder surgery and sports medicine. Prior to coming to Wellstar, Dr Burns was a leader at the prestigious Southern California Orthopedic Institute in Los Angeles, where he trained over 60 fellows and partnered with UCLA to provide world-class orthopedic care and research. Currently, he is on faculty with the Wellstar Kennestone Orthopedic Residency. He has been selected as a Master Arthroscopic Surgeon and a Top Doc in his region every year since 2010.
Dr Burns provides comprehensive surgical care, including but not limited to arthroscopic rotator cuff tendon repair, labral repair, shoulder replacement, “reverse” shoulder replacement, shoulder fracture care.
As a former athlete turned orthopedic surgeon, Dr. Burns uses his skills to help people with injuries or degenerative conditions live a healthy, active life.
In his practice, Dr. Burns’ professional mission is to provide a respectful, personalized and expert healthcare experience for each and every person. That means he works with patients to find the best treatment options for their orthopedic needs, whether it requires surgery or not.
Dr. Burns is a dedicated health partner on his patients’ journey to wellness, from injury to surgery and all the way through recovery. Through his work, he helps patients regain mobility, overcome pain and get back to enjoying life.
Specialties
- Orthopedic Surgery
Education & Training
- Georgetown University School of Medicine
Degree
- Doctor of Medicine
Residency
- University of Connecticut
Fellowship
- Southern California Orthopedic Institute
Certifications
- American Board of Orthopaedic Surgery
Hospital Affiliations
- Wellstar Spalding Regional Hospital
- Wellstar North Fulton Hospital
- Wellstar Windy Hill Hospital
- Wellstar Paulding Medical Center
- Wellstar Cobb Hospital
- Wellstar Douglas Hospital
- Wellstar Kennestone Hospital
- Wellstar West Georgia Medical Center
Languages spoken
- English
Patient Reviews
Overall patient rating
4.8Based on 301 patient ratings
- I'd recommend this practice to family and friends
-
- I'd recommend this provider to family and friends
-
- Listened to me carefully
-
- Earned my trust
-
- Shared the right amount of information
-
All reviews have been submitted by patients after seeing the provider.For more information about the review system, check out this Learn more about our review system.
Patient Reviews
5
It would be wonderful if all doctors were as informative as Dr. Burns. It is a joy meeting with him and understanding my situation. He is one of the best doctors I enjoy my visit with him. My son came with me, he said to me that Dr. Burns is as informative and understanding as any doctors he has known since living in the Roswell area. Doctor Burns enjoy your visits back to Stamford, Conn.
March 4, 2026
5
The nurses were very nice and accommodating. Doctor Burns explained the future of my treatment.
March 4, 2026
5
Dr. Burns...great visit, very informative, appreciated answers to all my questions I didn't need to ask!
February 26, 2026
5
I am a brand new patient for Dr Joseph Burns. I had a very POSITIVE , professional and focused in me appt from Dr Burns , and every staff member I interacted with from X ray technician( she's fabulous!) to his caring and kind PA to my very personable and informative diagnosis and treatment plan with my doctor. Appreciated all the written documentation on PT specific process I was prescribed. PS- no long wait and wait and wait either! And... I've already sent his contact information to a friend! I look forward to my shoulder getting stronger and healing under Dr Joseph Burns' care.
February 21, 2026
5
Wonderful experience.
February 20, 2026
5
Very pleasant and professional.
February 19, 2026
5
Very friendly staff, informative
February 19, 2026
5
Efficient and professional staff. Great environment, made me feel comfortable throughout the process . Gave me clear explanations of the procedure and diagnosis.
February 18, 2026
5
Everyone of the staff members went above and beyond when it came to delivering great service..... One of the best experiences.. thank you
February 18, 2026
5
Staff were absolutely attentive to all of my concerns
February 18, 2026
5
Dr. Burns listened to my concerns and took the time to evaluate me and recommend next steps. I highly recommend him.
February 15, 2026
5
Great provider who listens to his patients.
February 14, 2026
4
Dr was excellent ! X-ray tech was not so friendly
February 12, 2026
5
Great Dr and staff and experience. They set the bar high for others!
January 30, 2026
5
Professional culture by all in the practice. Excellent experience.
January 28, 2026
5
From the front desk staff, to the nurse, and to Dr Burns, they all made me feel valued and I so appreciate how they treated me with such kindness and respect.
January 28, 2026
4
We thought he was very good the first time we ever met him. He's very difficult to get into, probably because he is good. And you can tell sometimes where he's a little rushed and that's kind of how we felt last time. But ultimately, we very much trust him for his care with my mom. And he's worth the wait. Thank you.
January 17, 2026
5
Staff was able to work me in after visit to ER about week before initial appointment. Greatly appreciated.
January 16, 2026
5
Everyone is very pleasant and willing to help in the best way they can.
January 14, 2026
4
This was my first visit at this practice, so I hesitate to make a quick judgment about any of the questions you asked.
December 5, 2025
5
extremely professional, knowledgeable, and caring.
December 4, 2025
5
Dr. Burns is always very thorough, he answers all my questions and explains everything so I understand.
November 17, 2025
5
Upper Hembree office closed. Saw Dr Burns at Wellstar Urgent. Care LL1 Not Upper Hembree
November 15, 2025
5
Dr Burns excellent We are fortunate to have him at Wellstar.
November 15, 2025
5
all was fine...great staff. dr, burns and his NP are outstanding
November 1, 2025
5
The team was wonderful. They took care of me like I was a member of the family. I was really, really happy with the attention that I received, the explanations that I got, and how well I was handled. That sounds bad, but I mean their handling of me as a patient. There was a slight delay, but when they realized I'd been waiting a while, they were very apologetic and took care of me straight away. So I'm very happy and I would definitely recommend your practice. Thank you.
November 2, 2025
5
Great team
October 24, 2025
5
Dr. Joseph Burns and PA Jennie McCarthy have been superb. From my initial appointment, my surgery, throughout my physical therapy and recovery, they have provided excellent care and feedback. I am thankful to have them as my medical team.
October 23, 2025
5
Incredible experience with Dr Burns and his team. Highly recommend to anyone in need.
October 16, 2025
5
This practice is wonderful, I have no complaints.
October 15, 2025
5
It would be wonderful if all doctors were as informative as Dr. Burns. It is a joy meeting with him and understanding my situation. He is one of the best doctors I enjoy my visit with him. My son came with me, he said to me that Dr. Burns is as informative and understanding as any doctors he has known since living in the Roswell area. Doctor Burns enjoy your visits back to Stamford, Conn.
March 4, 2026
5
The nurses were very nice and accommodating. Doctor Burns explained the future of my treatment.
March 4, 2026
5
Dr. Burns...great visit, very informative, appreciated answers to all my questions I didn't need to ask!
February 26, 2026
5
I am a brand new patient for Dr Joseph Burns. I had a very POSITIVE , professional and focused in me appt from Dr Burns , and every staff member I interacted with from X ray technician( she's fabulous!) to his caring and kind PA to my very personable and informative diagnosis and treatment plan with my doctor. Appreciated all the written documentation on PT specific process I was prescribed. PS- no long wait and wait and wait either! And... I've already sent his contact information to a friend! I look forward to my shoulder getting stronger and healing under Dr Joseph Burns' care.
February 21, 2026
5
Wonderful experience.
February 20, 2026
5
Very pleasant and professional.
February 19, 2026
5
Very friendly staff, informative
February 19, 2026
5
Efficient and professional staff. Great environment, made me feel comfortable throughout the process . Gave me clear explanations of the procedure and diagnosis.
February 18, 2026
5
Everyone of the staff members went above and beyond when it came to delivering great service..... One of the best experiences.. thank you
February 18, 2026
5
Staff were absolutely attentive to all of my concerns
February 18, 2026
5
Dr. Burns listened to my concerns and took the time to evaluate me and recommend next steps. I highly recommend him.
February 15, 2026
5
Great provider who listens to his patients.
February 14, 2026
5
Great Dr and staff and experience. They set the bar high for others!
January 30, 2026
5
Professional culture by all in the practice. Excellent experience.
January 28, 2026
5
From the front desk staff, to the nurse, and to Dr Burns, they all made me feel valued and I so appreciate how they treated me with such kindness and respect.
January 28, 2026
5
Staff was able to work me in after visit to ER about week before initial appointment. Greatly appreciated.
January 16, 2026
5
Everyone is very pleasant and willing to help in the best way they can.
January 14, 2026
5
extremely professional, knowledgeable, and caring.
December 4, 2025
5
Dr. Burns is always very thorough, he answers all my questions and explains everything so I understand.
November 17, 2025
5
Upper Hembree office closed. Saw Dr Burns at Wellstar Urgent. Care LL1 Not Upper Hembree
November 15, 2025
5
Dr Burns excellent We are fortunate to have him at Wellstar.
November 15, 2025
5
all was fine...great staff. dr, burns and his NP are outstanding
November 1, 2025
5
The team was wonderful. They took care of me like I was a member of the family. I was really, really happy with the attention that I received, the explanations that I got, and how well I was handled. That sounds bad, but I mean their handling of me as a patient. There was a slight delay, but when they realized I'd been waiting a while, they were very apologetic and took care of me straight away. So I'm very happy and I would definitely recommend your practice. Thank you.
November 2, 2025
5
Great team
October 24, 2025
5
Dr. Joseph Burns and PA Jennie McCarthy have been superb. From my initial appointment, my surgery, throughout my physical therapy and recovery, they have provided excellent care and feedback. I am thankful to have them as my medical team.
October 23, 2025
5
Incredible experience with Dr Burns and his team. Highly recommend to anyone in need.
October 16, 2025
5
This practice is wonderful, I have no complaints.
October 15, 2025
4
Dr was excellent ! X-ray tech was not so friendly
February 12, 2026
4
We thought he was very good the first time we ever met him. He's very difficult to get into, probably because he is good. And you can tell sometimes where he's a little rushed and that's kind of how we felt last time. But ultimately, we very much trust him for his care with my mom. And he's worth the wait. Thank you.
January 17, 2026
4
This was my first visit at this practice, so I hesitate to make a quick judgment about any of the questions you asked.
December 5, 2025
4
Dr was excellent ! X-ray tech was not so friendly
February 12, 2026
4
We thought he was very good the first time we ever met him. He's very difficult to get into, probably because he is good. And you can tell sometimes where he's a little rushed and that's kind of how we felt last time. But ultimately, we very much trust him for his care with my mom. And he's worth the wait. Thank you.
January 17, 2026
4
This was my first visit at this practice, so I hesitate to make a quick judgment about any of the questions you asked.
December 5, 2025
5
It would be wonderful if all doctors were as informative as Dr. Burns. It is a joy meeting with him and understanding my situation. He is one of the best doctors I enjoy my visit with him. My son came with me, he said to me that Dr. Burns is as informative and understanding as any doctors he has known since living in the Roswell area. Doctor Burns enjoy your visits back to Stamford, Conn.
March 4, 2026
5
The nurses were very nice and accommodating. Doctor Burns explained the future of my treatment.
March 4, 2026
5
Dr. Burns...great visit, very informative, appreciated answers to all my questions I didn't need to ask!
February 26, 2026
5
I am a brand new patient for Dr Joseph Burns. I had a very POSITIVE , professional and focused in me appt from Dr Burns , and every staff member I interacted with from X ray technician( she's fabulous!) to his caring and kind PA to my very personable and informative diagnosis and treatment plan with my doctor. Appreciated all the written documentation on PT specific process I was prescribed. PS- no long wait and wait and wait either! And... I've already sent his contact information to a friend! I look forward to my shoulder getting stronger and healing under Dr Joseph Burns' care.
February 21, 2026
5
Wonderful experience.
February 20, 2026
5
Very pleasant and professional.
February 19, 2026
5
Very friendly staff, informative
February 19, 2026
5
Efficient and professional staff. Great environment, made me feel comfortable throughout the process . Gave me clear explanations of the procedure and diagnosis.
February 18, 2026
5
Everyone of the staff members went above and beyond when it came to delivering great service..... One of the best experiences.. thank you
February 18, 2026
5
Staff were absolutely attentive to all of my concerns
February 18, 2026
5
Dr. Burns listened to my concerns and took the time to evaluate me and recommend next steps. I highly recommend him.
February 15, 2026
5
Great provider who listens to his patients.
February 14, 2026
5
Great Dr and staff and experience. They set the bar high for others!
January 30, 2026
5
Professional culture by all in the practice. Excellent experience.
January 28, 2026
5
From the front desk staff, to the nurse, and to Dr Burns, they all made me feel valued and I so appreciate how they treated me with such kindness and respect.
January 28, 2026
5
Staff was able to work me in after visit to ER about week before initial appointment. Greatly appreciated.
January 16, 2026
5
Everyone is very pleasant and willing to help in the best way they can.
January 14, 2026
5
extremely professional, knowledgeable, and caring.
December 4, 2025
5
Dr. Burns is always very thorough, he answers all my questions and explains everything so I understand.
November 17, 2025
5
Upper Hembree office closed. Saw Dr Burns at Wellstar Urgent. Care LL1 Not Upper Hembree
November 15, 2025
5
Dr Burns excellent We are fortunate to have him at Wellstar.
November 15, 2025
5
all was fine...great staff. dr, burns and his NP are outstanding
November 1, 2025
5
The team was wonderful. They took care of me like I was a member of the family. I was really, really happy with the attention that I received, the explanations that I got, and how well I was handled. That sounds bad, but I mean their handling of me as a patient. There was a slight delay, but when they realized I'd been waiting a while, they were very apologetic and took care of me straight away. So I'm very happy and I would definitely recommend your practice. Thank you.
November 2, 2025
5
Great team
October 24, 2025
5
Dr. Joseph Burns and PA Jennie McCarthy have been superb. From my initial appointment, my surgery, throughout my physical therapy and recovery, they have provided excellent care and feedback. I am thankful to have them as my medical team.
October 23, 2025
5
Incredible experience with Dr Burns and his team. Highly recommend to anyone in need.
October 16, 2025
5
This practice is wonderful, I have no complaints.
October 15, 2025
5
It would be wonderful if all doctors were as informative as Dr. Burns. It is a joy meeting with him and understanding my situation. He is one of the best doctors I enjoy my visit with him. My son came with me, he said to me that Dr. Burns is as informative and understanding as any doctors he has known since living in the Roswell area. Doctor Burns enjoy your visits back to Stamford, Conn.
March 4, 2026
5
The nurses were very nice and accommodating. Doctor Burns explained the future of my treatment.
March 4, 2026
5
Dr. Burns...great visit, very informative, appreciated answers to all my questions I didn't need to ask!
February 26, 2026
5
I am a brand new patient for Dr Joseph Burns. I had a very POSITIVE , professional and focused in me appt from Dr Burns , and every staff member I interacted with from X ray technician( she's fabulous!) to his caring and kind PA to my very personable and informative diagnosis and treatment plan with my doctor. Appreciated all the written documentation on PT specific process I was prescribed. PS- no long wait and wait and wait either! And... I've already sent his contact information to a friend! I look forward to my shoulder getting stronger and healing under Dr Joseph Burns' care.
February 21, 2026
5
Wonderful experience.
February 20, 2026
5
Very pleasant and professional.
February 19, 2026
5
Very friendly staff, informative
February 19, 2026
5
Efficient and professional staff. Great environment, made me feel comfortable throughout the process . Gave me clear explanations of the procedure and diagnosis.
February 18, 2026
5
Everyone of the staff members went above and beyond when it came to delivering great service..... One of the best experiences.. thank you
February 18, 2026
5
Staff were absolutely attentive to all of my concerns
February 18, 2026
5
Dr. Burns listened to my concerns and took the time to evaluate me and recommend next steps. I highly recommend him.
February 15, 2026
5
Great provider who listens to his patients.
February 14, 2026
4
Dr was excellent ! X-ray tech was not so friendly
February 12, 2026
5
Great Dr and staff and experience. They set the bar high for others!
January 30, 2026
5
Professional culture by all in the practice. Excellent experience.
January 28, 2026
5
From the front desk staff, to the nurse, and to Dr Burns, they all made me feel valued and I so appreciate how they treated me with such kindness and respect.
January 28, 2026
4
We thought he was very good the first time we ever met him. He's very difficult to get into, probably because he is good. And you can tell sometimes where he's a little rushed and that's kind of how we felt last time. But ultimately, we very much trust him for his care with my mom. And he's worth the wait. Thank you.
January 17, 2026
5
Staff was able to work me in after visit to ER about week before initial appointment. Greatly appreciated.
January 16, 2026
5
Everyone is very pleasant and willing to help in the best way they can.
January 14, 2026
4
This was my first visit at this practice, so I hesitate to make a quick judgment about any of the questions you asked.
December 5, 2025
5
extremely professional, knowledgeable, and caring.
December 4, 2025
5
Dr. Burns is always very thorough, he answers all my questions and explains everything so I understand.
November 17, 2025
5
Upper Hembree office closed. Saw Dr Burns at Wellstar Urgent. Care LL1 Not Upper Hembree
November 15, 2025
5
Dr Burns excellent We are fortunate to have him at Wellstar.
November 15, 2025
5
The team was wonderful. They took care of me like I was a member of the family. I was really, really happy with the attention that I received, the explanations that I got, and how well I was handled. That sounds bad, but I mean their handling of me as a patient. There was a slight delay, but when they realized I'd been waiting a while, they were very apologetic and took care of me straight away. So I'm very happy and I would definitely recommend your practice. Thank you.
November 2, 2025
5
all was fine...great staff. dr, burns and his NP are outstanding
November 1, 2025
5
Great team
October 24, 2025
5
Dr. Joseph Burns and PA Jennie McCarthy have been superb. From my initial appointment, my surgery, throughout my physical therapy and recovery, they have provided excellent care and feedback. I am thankful to have them as my medical team.
October 23, 2025
5
Incredible experience with Dr Burns and his team. Highly recommend to anyone in need.
October 16, 2025
5
This practice is wonderful, I have no complaints.
October 15, 2025
5
This practice is wonderful, I have no complaints.
October 15, 2025
5
Incredible experience with Dr Burns and his team. Highly recommend to anyone in need.
October 16, 2025
5
Dr. Joseph Burns and PA Jennie McCarthy have been superb. From my initial appointment, my surgery, throughout my physical therapy and recovery, they have provided excellent care and feedback. I am thankful to have them as my medical team.
October 23, 2025
5
Great team
October 24, 2025
5
all was fine...great staff. dr, burns and his NP are outstanding
November 1, 2025
5
The team was wonderful. They took care of me like I was a member of the family. I was really, really happy with the attention that I received, the explanations that I got, and how well I was handled. That sounds bad, but I mean their handling of me as a patient. There was a slight delay, but when they realized I'd been waiting a while, they were very apologetic and took care of me straight away. So I'm very happy and I would definitely recommend your practice. Thank you.
November 2, 2025
5
Dr Burns excellent We are fortunate to have him at Wellstar.
November 15, 2025
5
Upper Hembree office closed. Saw Dr Burns at Wellstar Urgent. Care LL1 Not Upper Hembree
November 15, 2025
5
Dr. Burns is always very thorough, he answers all my questions and explains everything so I understand.
November 17, 2025
5
extremely professional, knowledgeable, and caring.
December 4, 2025
4
This was my first visit at this practice, so I hesitate to make a quick judgment about any of the questions you asked.
December 5, 2025
5
Everyone is very pleasant and willing to help in the best way they can.
January 14, 2026
5
Staff was able to work me in after visit to ER about week before initial appointment. Greatly appreciated.
January 16, 2026
4
We thought he was very good the first time we ever met him. He's very difficult to get into, probably because he is good. And you can tell sometimes where he's a little rushed and that's kind of how we felt last time. But ultimately, we very much trust him for his care with my mom. And he's worth the wait. Thank you.
January 17, 2026
5
From the front desk staff, to the nurse, and to Dr Burns, they all made me feel valued and I so appreciate how they treated me with such kindness and respect.
January 28, 2026
5
Professional culture by all in the practice. Excellent experience.
January 28, 2026
5
Great Dr and staff and experience. They set the bar high for others!
January 30, 2026
4
Dr was excellent ! X-ray tech was not so friendly
February 12, 2026
5
Great provider who listens to his patients.
February 14, 2026
5
Dr. Burns listened to my concerns and took the time to evaluate me and recommend next steps. I highly recommend him.
February 15, 2026
5
Staff were absolutely attentive to all of my concerns
February 18, 2026
5
Efficient and professional staff. Great environment, made me feel comfortable throughout the process . Gave me clear explanations of the procedure and diagnosis.
February 18, 2026
5
Everyone of the staff members went above and beyond when it came to delivering great service..... One of the best experiences.. thank you
February 18, 2026
5
Very friendly staff, informative
February 19, 2026
5
Very pleasant and professional.
February 19, 2026
5
Wonderful experience.
February 20, 2026
5
I am a brand new patient for Dr Joseph Burns. I had a very POSITIVE , professional and focused in me appt from Dr Burns , and every staff member I interacted with from X ray technician( she's fabulous!) to his caring and kind PA to my very personable and informative diagnosis and treatment plan with my doctor. Appreciated all the written documentation on PT specific process I was prescribed. PS- no long wait and wait and wait either! And... I've already sent his contact information to a friend! I look forward to my shoulder getting stronger and healing under Dr Joseph Burns' care.
February 21, 2026
5
Dr. Burns...great visit, very informative, appreciated answers to all my questions I didn't need to ask!
February 26, 2026
5
The nurses were very nice and accommodating. Doctor Burns explained the future of my treatment.
March 4, 2026
5
It would be wonderful if all doctors were as informative as Dr. Burns. It is a joy meeting with him and understanding my situation. He is one of the best doctors I enjoy my visit with him. My son came with me, he said to me that Dr. Burns is as informative and understanding as any doctors he has known since living in the Roswell area. Doctor Burns enjoy your visits back to Stamford, Conn.
March 4, 2026
Publications and Articles


Advancements in orthopedic care
This article was originally published on Atlanta Business Chronicle on April 12, 2024.
Orthopedic care has evolved from injury treatment and corrective surgery into a critical component of modern healthcare. As primary care remains foundational in managing overall health, the demand for orthopedic services has surged, reflecting changing lifestyles, demographics and expectations. In any given year, 12% to 14% of the adult population will visit their physician for back pain, according to the United States Bone and Joint Initiative (USBJI).
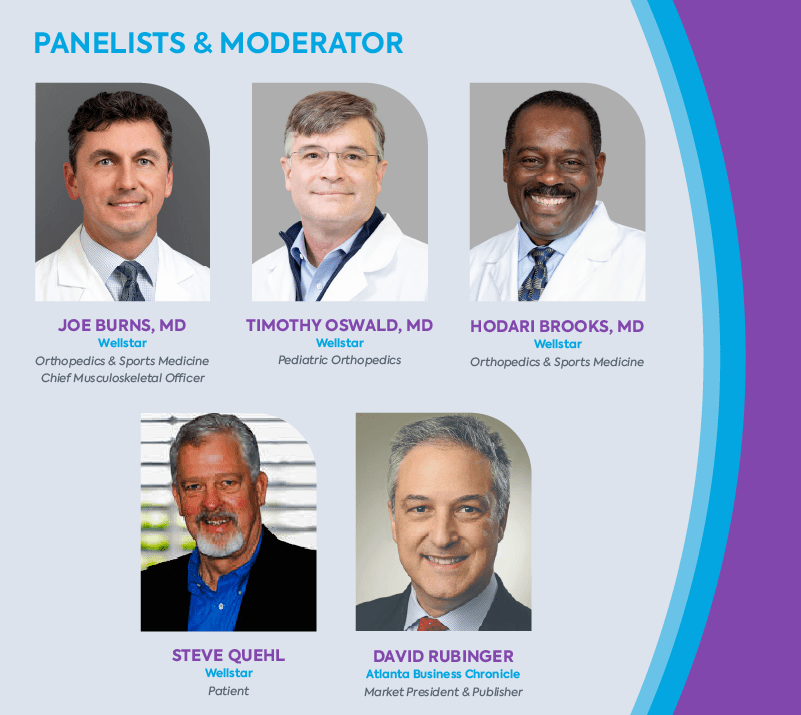
Against this backdrop of widespread musculoskeletal issues, Wellstar recently convened with the Atlanta Business Chronicle for a panel discussion to delve into the changing landscape of orthopedic care. This insightful forum explored key trends, challenges and innovations shaping the field, with leading healthcare professionals offering valuable perspectives. These discussions unraveled the complexities of orthopedic care, ranging from preventive strategies to cutting-edge treatments. Among the panelists was Steve Quehl, a former college football player for Notre Dame, who started as a tight end before transitioning to a center. Other panelists were Dr. Hodari Brooks, orthopedic surgeon, Wellstar Health System; Dr. Joseph Burns, chief musculoskeletal officer, Wellstar Health System; Dr. Timothy Oswald, pediatric orthopedic surgeon, Wellstar Pediatric Orthopedics. Moderator was David Rubinger, market president and publisher, Atlanta Business Chronicle.
The rise of orthopedics and interventions
David Rubinger: There’s an uptick in the demand for orthopedic services and these specialists have become increasingly essential to healthcare. What societal changes drive this heightened need for specialized ortho care?
Dr. Joseph Burns: We’re facing an aging population alongside a growing desire for an active, pain-free lifestyle. In the past, individuals had to endure their limitations and pain for life. Today, people have more options. Technology, techniques and training advancements now provide surgical alternatives that significantly enhance quality of life well beyond middle age.
Wellstar conducts numerous community campaigns through various channels, including community events, the media and in our offices and hospitals, highlighting the value of maintaining health and establishing a relationship with a primary care physician.
Dr. Hodari Brooks: Societal changes for both our youth as well as adults have resulted in the increased need for orthopedic care. Physical activity has decreased, with fewer kids participating in physical education. This leads to more injuries related to obesity and lack of activity. The need for joint replacements is soaring, driven by both baby boomers aging and younger individuals seeking treatment earlier. Half of my practice is caring for patients under 55, a shift from when people would wait years for treatment. Now, we prioritize improving quality of life sooner rather than later.
Patients, including those seeking joint replacements, are opting for earlier interventions. They are less inclined to wait for treatment, indicating a shift within the healthcare system towards promptly addressing patient needs.
Rubinger: What new injury trends are emerging in sports due to changing physical activity patterns, especially with the rise of extreme sports and diverse workout routines?
Dr. Burns: The rise in overuse injuries among our younger population is disheartening. Young athletes don’t diversify their sports as they once did, leading to year-round specialization and an increased risk of injury. This relentless pursuit of success often comes at the cost of rest and diversity in physical activities.
We’re also encountering complex medical issues that require specialized treatment, reflecting both advancements in medical care and the aging population’s evolving healthcare needs. Conditions once considered untreatable are now within our reach, marking a significant shift in the scope of orthopedic care over the years.
Rubinger: Dr. Oswald, as a pediatric orthopedic specialist, have you frequently observed the concept of subspecialization and the decline in diversification among young athletes?
Dr. Timothy Oswald: It’s a significant area of concern for us, and we’re conducting more research. Recent studies have highlighted the insufficient breaks and rest periods given to children, as well as the trend of starting high-level athletics too young, which aligns with the issue of subspecialization. Kids are not miniature adults. Their orthopedic stresses differ due to growth plates and differing stress responses.
We’re educating the community, including coaches and parents, about the importance of rest periods during training through channels like social media. We aim to implement better training methods so young athletes can continue playing into their college years, as we’re noticing a concerning trend where many high-level athletes quit sports as early as eighth grade.
Rubinger: Steve, as a former college athlete yourself, what’s your observation of the sports world’s changes regarding how injuries are approached, especially compared to when we were younger?
Steve Quehl: I view this issue through the lens of my grandchildren and their friends, and I agree with the insights shared by these doctors. Their perspectives must influence parents’ decisions, particularly regarding the early specialization trend. Parents often have unrealistic expectations of their children becoming professional athletes, which can lead to overtraining and injuries. Kids should have a balanced approach to sports. I’m grateful my daughters chose activities like swimming over contact sports for their children, considering the risks to growing bones and muscles.
Prior to my enrollment at Notre Dame, I appreciated the joy of playing multiple sports during each season for fun, without the pressure of turning it into a professional pursuit.
Efficient outpatient care benefits
Rubinger: I’ve noticed remarkable changes in my lifetime regarding the duration of procedures and the efficiency of hospital stays or visits to outpatient surgery centers. I’m curious about your perspective on this shift away from extended hospital stays. Do you believe it’s ultimately beneficial or detrimental to patients? What are your thoughts on this evolution of the time spent in hospitals or surgery centers?
Dr. Brooks: There’s been a significant shift in the duration of hospital stays, especially concerning joint procedures. In the past, patients would typically spend several days in the hospital before and after surgery. In my practice, around 90% of primary joint patients can return home the same day, which is remarkable. This change is not only due to patient preferences for quicker recovery but also has medical benefits, such as reducing the risk of infection. Outpatient joint replacement is not done everywhere, however, and it is important to discuss this option with your individual surgeon.
Insurance companies have started incentivizing shorter hospital stays. While this trend has clear advantages, it also comes with challenges, such as pressure to discharge patients quickly. The ability to expedite recovery and minimize specific complications is a positive development I believe will continue.
Rubinger: Do we have data showing a decrease in complications due to the trend of shorter hospital stays, particularly for joint procedures?
Dr. Burns: Evidence indicates improved outcomes for outpatient procedures, with data supporting this trend. The shift involves a comprehensive approach beyond simply performing the surgery and discharging the patient. It requires a multidisciplinary effort, with investments in establishing preoperative optimization programs, patient education classes and a coordinated team approach on the day of surgery.
Patients undergo physical therapy before returning home, but the care doesn’t stop there. We must ensure effective pain management, minimize infection risks and create a safe home environment to support their recovery. This process goes beyond safely discharging patients. It’s about ensuring their complete and safe recovery. I’m proud of the extensive teamwork and complex processes that Wellstar has implemented to support these programs.
Quehl: When it was time to correct my right shoulder this past year, I went in the morning and came back home in the evening. Dr. Burns assured me that I’d be home the same day, and it was a wonderful experience. I didn’t want any overnight stays. It was well-planned and executed, with proper anticipation and expectations set. The follow-up was excellent, too.
Dr. Brooks: Patients are shocked or hesitant when I inform them that they’ll go home the same day. It’s about managing expectations and explaining the benefits, especially as it relates to improved outcomes. Involvement in these programs gives physicians more control over the process. It’s a serious undertaking but rewarding because we can provide more input, especially in an outpatient setting. Collaboration with anesthesia colleagues has improved, particularly with techniques like regional blocks, as patients need to be up and about after surgery. Almost universally in my experience, patients prefer their outpatient surgical experience to any previous hospital stays.
Multimodal pain management success
Rubinger: This leads me to my next question regarding opioids and pharmacology. Has pharmacology evolved over the last decade to improve patient treatment?
Dr. Burns: Most of us are employing what we refer to as multimodal pain control, which involves a process aimed at sparing, if not entirely eliminating, the need for opioids as a primary method of pain management. By utilizing different medications that target distinct pain receptors, we can effectively manage pain while minimizing potential side effects that may arise from relying solely on opioids or multiple doses of the same medication. Advancements in regional blocks, administered by anesthesiologists, allow injections that can provide numbing effects in the affected areas for several days, alleviating initial post-operative pain and reducing patients’ overall need for pain medication over time.
Dr. Oswald: The opioid crisis in the greater Atlanta area is a significant concern for both children and adults, and it’s something we’re all acutely aware of. We’ve initiated extensive research efforts at Wellstar to address this issue and lead advancements in pain management that don’t rely on narcotics. Similar to the approach described in the total joint experience, we’ve been observing this trend for some time now, even in pediatric cases.
When I trained for pediatric spine surgery 20 years ago, patients stayed in the hospital for at least a week post-surgery. By implementing multimodal approaches, we’ve managed to reduce narcotic use by nearly 90% while also transitioning from a week-long hospital stay to just a 23-hour observation period for certain procedures.
Patient satisfaction is higher with these approaches, directly correlating with their overall experience. Are we expediting discharge solely for the sake of pushing people out? Actually, no. It’s about ensuring patients feel empowered in their recovery process, with their pain managed effectively, and their ability to return to the quality of life they desire. These patient-centered care programs optimize outcomes and enhance the overall healthcare experience.

Joseph Burns, MD

Orthopedic Surgeon with Wellstar since 2020
Rating
4.8
|
|
Specialties
Orthopedic Surgery
Education
Doctor of Medicine
Medical School
Georgetown University School of Medicine
Residency
University of Connecticut
Fellowship
Southern California Orthopedic Institute
Certifications
American Board of Orthopaedic Surgery
Spoken Languages
English
Hospital Affiliations
Wellstar Spalding Regional Hospital Wellstar North Fulton Hospital Wellstar Windy Hill Hospital Wellstar Paulding Medical Center Wellstar Cobb Hospital Wellstar Douglas Hospital Wellstar Kennestone Hospital Wellstar West Georgia Medical Center
Office Locations
|
|
www.wellstar.org/physicians/joseph-burns-md
|
We use cookies for booking and general analytics. Learn more about or internet privacy policy.

