Wellstar knows that the beginning of the school year is often accompanied by getting back to extracurricular activities. With the return to the classroom and competition arenas, we know parents, coaches and teachers alike are concerned that their student athletes are fueling their bodies and brains for optimal performance.
Wellstar Pediatric Orthopedics recommends getting the correct amount of protein, carbohydrates, healthy fats, iron, calcium and vitamin D, as well as fluids. Dietary supplements are not needed for youth athletes unless recommended by a healthcare professional. It is more important to meet the body’s caloric needs.
For hydration, it’s recommended that student athletes consume up to 20 ounces of fluid one hour before an activity and 5 ounces every 15 minutes during the activity.
“Proper nutrition and hydration are critical for all students, but particularly for athletes who are more active and burning more calories,” said Dr. Lindsay Stephenson, Wellstar pediatric orthopedic surgeon and sports medicine specialist. “I recommend using the nutritional guide released by the Pediatric Orthopaedic Society of North America. This information makes it easier for students and their parents to understand the nutritional needs of the body to perform in the classroom and during competition.”
Access the recommended nutritional guide.
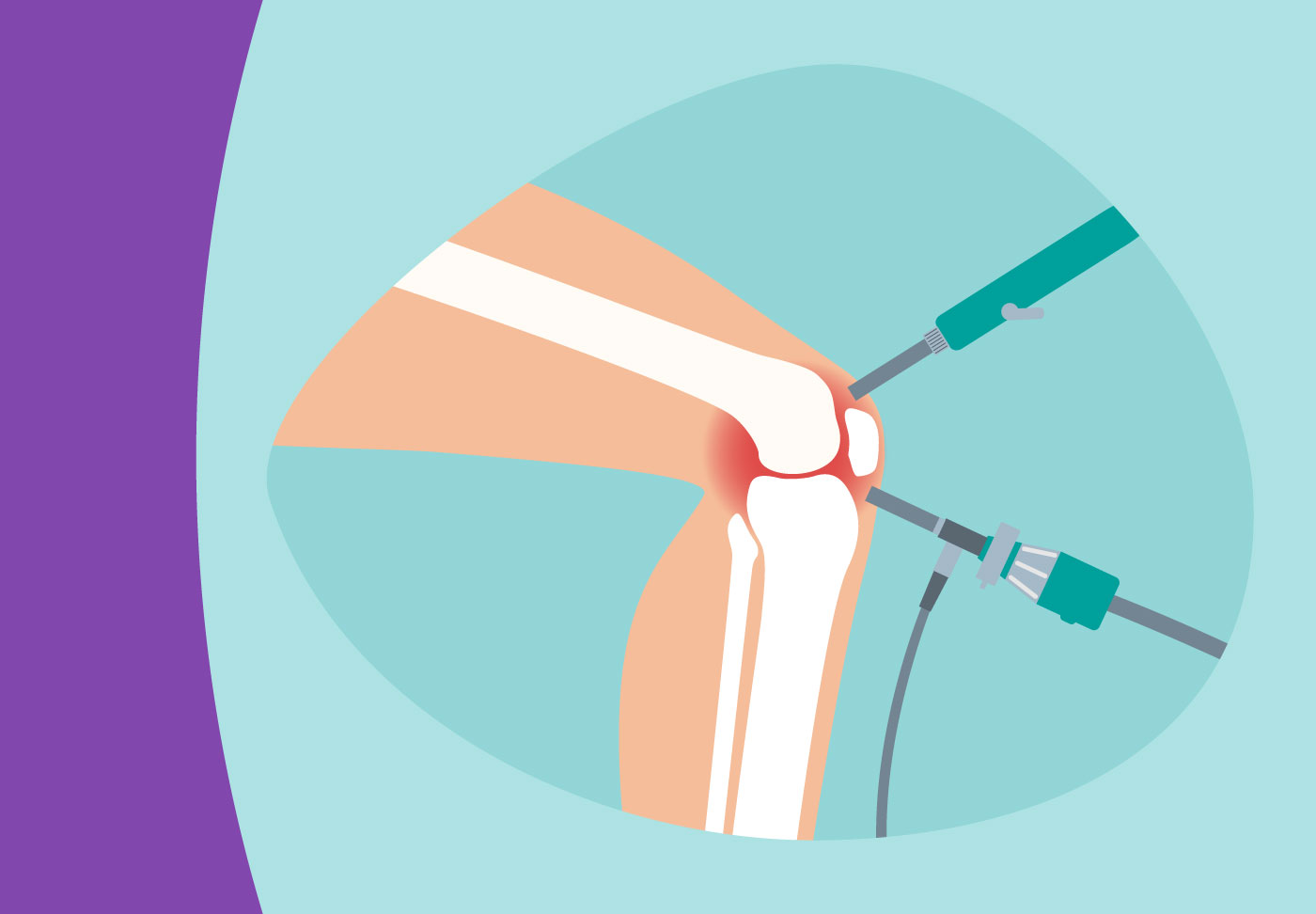
To learn more or make an appointment with Wellstar Pediatric Orthopedics, visit wellstar.org/pedsortho.