This article was originally published on Atlanta Business Chronicle on July 14, 2023.
The key to avoiding health problems is prevention, and the keys to prevention are annual checkups, regular screenings and vaccinations. With the start of the next school year looming in late summer, healthcare experts in Atlanta say it’s a good time for families to get back into the routine of scheduling and keeping these important appointments—not just for children, but for parents too, especially that one parent who tends to be the primary scheduler, often the mother.
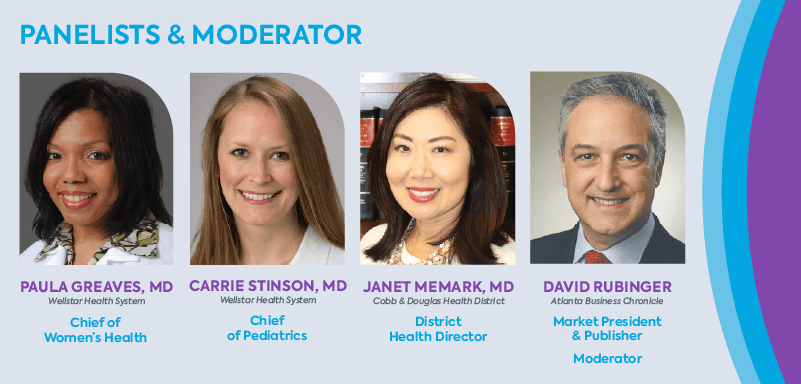
In an Atlanta Business Chronicle panel discussion in partnership with Wellstar, physicians from Wellstar and Cobb & Douglas Health District discuss why checkups are important and how families can overcome obstacles to stay on track with preventative care.
Taking care of the family and the family’s No. 1 manager
David Rubinger, Atlanta Business Chronicle market president and publisher: When we think about family wellness and how it intersects with our daily work routines, it can get very complicated, given how busy working professionals are. We’re trying to figure out a way to manage not only our children’s health, and maybe our parents’ health if we’re in the sandwich generation, but our own health. The checklist is longer and longer every day. Let’s start with the basics. We’re a few weeks away from the start of school. Dr. Stinson, what are you telling your parents of kids of school age right now?
Dr. Carrie Stinson, Chief, Pediatric Service Line, Wellstar: The summer is a great time to get caught up on all the things that fall through the cracks during the busy school year. Our lives are very hectic, and when school starts back, things get even busier.
One big thing is the annual well-child exam. Every child should have a well-child exam every single year. When you have babies and toddlers, it’s routine — you’re scheduling these frequently. When kids get older and busier, these visits may feel less important and fall off your radar.
Well visits are important every year. They focus on the comprehensive health and well-being of your child. Pediatricians focus on physical health, development, emotional, social, and even behavioral health. During these visits, the care team collects information on patient and family history, talks about developmental milestones and how your child is doing in school socially. We also assess sleep habits and nutrition. As they become adolescents, well-child exams become even more important as we ask questions about your child’s mental and sexual health.
Those are important conversations to start having and your pediatrician can be a great facilitator. Sometimes parents are uncomfortable talking about those topics with their children even at an early, pre-adolescent stage, so those well checkups are really great places to get insight on how to approach sensitive topics.
Rubinger: Dr. Stinson, since COVID, tell me what you’re seeing that’s different in terms of talking to both parents and children. I am sure the pandemic took some families off their schedules for well checkups. How has the doctor-patient pediatric conversation changed over the past couple of years?
Dr. Stinson: What we’re hearing from our pediatricians since COVID is also what we’re hearing in the news. The behavioral and mental health crisis that we’re experiencing in this country has been really impactful on children, especially teenagers. During COVID, the social isolation of being out of school for periods of time had a significant impact on adolescents. The rise in social media popularity during that time also had a negative impact on pediatric mental health.
Our pediatricians are really seeing that impact now. They’re feeling the strain our teenagers are experiencing. We’re seeing many more cases of depression and anxiety, and cases that escalate to dangerous proportions such as suicidal thoughts and actions.
We’re trying to respond to it by increasing the resources in our communities, but it’s hard to move fast enough to keep up with the demand. At Wellstar, we are developing an integrative model for behavioral health into our pediatric offices. Five of our pediatric practices will have embedded behavioral health professionals, so pediatricians can make direct referrals and patients have immediate access to behavioral health providers in their pediatric office setting.
Rubinger: Dr. Greaves, the mother might be the caretaker who takes care of the child. Most mothers would put their kid’s health ahead of their own health. Tell me what you are experiencing in terms of women’s health as it relates to those people who are the caretakers. What are the issues that they’re having to face to address their own needs?
Dr. Paula Greaves, Chief, Women’s Health Service Line, Wellstar: Women are usually considered the CEOs of their households and the drivers of healthcare in the community. Most women are the care bridge between several generations. They take care of their children, their parents, their partners and at times their communities.
Unfortunately, they sometimes forget to take care of themselves. As physicians, it is our duty to ensure that women are made aware of the warning signs their bodies may be sending them and encourage them to seek help earlier to improve health outcomes.
There are nine signs that I tell my patients to watch out for:
- Fatigue: Most women think, “Oh, I’m tired. It’s because I’m doing too much or I’m not getting enough sleep.” But fatigue can be a sign of something more than simply lack of sleep. It could be thyroid dysfunction. It could be menstrual irregularities causing them to be anemic and thus feeling fatigued. It could be heart disease. Fatigue could also be a sign of depression or menopausal symptoms. Every household should own a blood pressure monitor, and women should know their numbers (blood pressure, weight, and last menstrual period).
- Women should be aware of physical changes within their bodies, including breast changes. Changes in the texture of the skin or a lump or pain in the breast should always be checked out.
- Bloating is another subtle symptom to be aware of. Most women feel bloated and think, “Oh, it’s time for my menstrual cycle, so that’s why I am bloated.” But bloating can be a sign of a gastrointestinal problem or an enlarged pelvic organ. If you have bloating that doesn’t resolve after one or two cycles, let your doctor know.
- Chest discomfort, shortness of breath and pain or discomfort in the jaw, neck, shoulder, or arm are also red flags. Heart attack signs and symptoms can be completely different in women than the typical ones seen in men. Heart disease is the number one killer of women, so it is very important that these signs are not ignored.
- Lung cancer isn’t just a smoker’s disease. If you notice an unusual cough or wheezing, have it checked out.
- Weight changes: Either too much weight gain or unexpected weight loss should be mentioned to your physician. Fluid retention can also affect weight gain.
- Blood in the urine or stool should be reported.
- Irregular or heavy periods—heavy enough to change pads every hour or soil through clothes.
- Skin changes such as discolorations, new moles or growths are definitely worth having a professional take a look.
Rubinger: Is there ever a situation, Dr. Stinson, where you are treating a child and you see a mother whom you can tell is having health issues, even without an exam? As a pediatrician, do you ever say, “Hey, I think you need to get that checked out?”
Dr. Stinson: As pediatricians, we really focus on the whole family. While we’re seeing the child, we’re also interacting with the parents, guardians, grandparents, or whoever’s bringing the child in to see us on a routine basis.
I think we often get questions from family members about their own health because of exactly what Dr. Greaves mentioned. People think, “I am in a doctor’s office. I don’t have time to go to my own doctor. Let me just see if I can get this question answered.
While being careful not to give medical advice to a patient who is not ours or who is outside of our scope of practice as pediatricians, we are very willing to give recommendations on where that person should seek care. One benefit of our health system is we have the expertise to take care of patients from before they’re born until they need end-of-life care. We have a scope of providers within our system who can help with pretty much any problem that might come up. I would not hesitate to refer a patient to Dr. Greaves and say, “This mom is really worried about her own health. Can you please help? She’s very busy, but her symptoms sound concerning. Can you maybe work her into your schedule?
I practice in the hospital, and we have sent several parents to the emergency room in our hospital for their own health while we’re taking care of their child in the pediatric unit.
How providers are addressing rising mental health needs
Rubinger: Dr. Memark, you get to look at this from the standpoint of two counties that are in great need of public health support. What are the trends that you’re seeing at a 30,000-foot view? What do you see within your communities that your organization tries to address?
Dr. Janet Memark, District Health Director, Cobb & Douglas Health District: From my point of view, one of the big things that we do at Cobb & Douglas Public Health is a large community health assessment. Dr. Greaves is actually a member of our board. We just finished a 2016-2020 five-year assessment. This was at the beginning of the pandemic, so keep that in mind. Our next assessment will capture 2021-2025. One of the things that was surprising to me was looking at causes of death in our communities. The assessment showed that in older people, it’s what you’d expect. For example, in Cobb County for those age 75 and older, the leading causes of death are things like vascular disease, stroke and Alzheimer’s. For ages 65 to 74, it’s heart disease and cancer. But when we started looking at the lower age groups, I was very surprised at what I saw:
- For people in their 30s and 40s, the leading cause of death was accidental poisonings, and that includes drug abuse and drug overdoses. Number two was suicide.
- For ages 25 to 34, number one was overdoses and poisonings and number two was suicide.
- For ages 20 to 24, motor vehicle accidents were number one. Suicide was also number two for this group.
- For 15 to 19, suicide took the number one spot. Number two was motor vehicle accidents.
- For 10 to 14, number one was motor vehicle accidents followed by suicide.
After the timeframe studied in the assessment, we went through two more years of the pandemic, which affected almost everyone’s mental health in one way or another. We’ve heard on the news how pediatricians in medical school are now being trained on how to provide more extensive mental healthcare because there just aren’t enough mental health experts.
It’s wonderful to hear Dr. Stinson say they are really trying to bolster up mental health screenings for our young people during their pediatric visits. I’d also like to add that we have high rates of maternal mortality in Georgia. The state Department of Public Health did a deep dive and found that mental health is a huge component of maternal mortality. You see these same themes of mental health running through several different medical specialties.