
Minimally Invasive Gynecological Surgery
A safer and more effective alternative to traditional open surgery for many gynecologic conditions.
Innovative Treatment to Optimize Recovery
Conditions & Treatments
- Robotic Surgery
- Endometriosis
- Fibroids
- Minimally Invasive Gynecology
- Robotic Hysterectomy
- Robotic Myomectomy
- Laparoscopic Hysterectomy
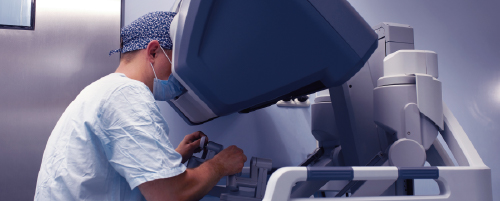
Robotic Surgery
Minimally invasive surgery has many advantages in comparison to open surgery, and using robot-assisted techniques refines the process even further. Nathan Mordel, MD, and the team at Wellstar Minimally Invasive Gynecological Surgery provide a selection of advanced minimally invasive robotic surgeries, including excision of endometriosis, sacrocolpopexy, and prophylactic removal of the fallopian tubes and ovaries.What is robotic surgery?
One in three women in the United States will have a hysterectomy before she turns 60. While no woman wants to face surgery, today the vast majority of gynecologic conditions -- from endometriosis to uterine fibroids and heavy menstrual bleeding to cancer -- can now be treated effectively without a big incision.With robot-assisted surgery, a hysterectomy requires only a few small incisions, so recovery is significantly less than the usual weeks required with traditional surgery. The da VinciⓇ Surgical System provides patients with minimally invasive surgical procedures that offer significant advantages over traditional “open” surgeries and advanced laparoscopic surgeries.
It improves the surgeon’s ergonomics, allows for three-dimensional (3D) visualization of the surgical field, and gives the surgeon superior control over the camera and instruments by mimicking his/her natural hand, wrist, and finger movements.
What are the advantages of robotic surgery?
Surgery with the da Vinci system enables gynecologists to perform the most precise, minimally invasive hysterectomy available today. For most women, da Vinci hysterectomy offers numerous potential benefits over traditional open surgery, including:- Significantly less pain
- Minimal blood loss and no need for transfusion
- Fewer complications
- Shorter hospital stay
- Quicker recovery and return to normal activities
- Small incisions for minimal scarring
- Better outcomes and patient satisfaction
What procedures are performed using robotic surgery?
Dr. Mordel routinely performs the following robot-assisted procedures using the da Vinci Surgical System:
- Prophylactic removal of tubes and ovaries
- Total hysterectomy
- Myomectomy
- Excision of endometriosis
- Excision of benign ovarian tumors
- Sacrocolpopexy
- Supracervical hysterectomy

Endometriosis
Endometriosis not only causes severe abdominal pain but can affect your chances of conceiving. If you’re experiencing heavy, painful periods, Nathan Mordel, MD, and the team at Wellstar Minimally Invasive Gynecological Surgery can find the cause and provide cutting-edge treatments to resolve the problem. They use the latest medical technologies and surgical techniques to treat endometriosis and are experts in performing robotic laparoscopic excision of endometriosis.
What is endometriosis?
Sometimes normal uterine lining (endometrial) cells seep through the fallopian tubes and implant into and proliferate through the inner coating of the pelvis (peritoneum). This results in different degrees of irritation of the pelvic peritoneum, causing pelvic pain. Such a phenomenon is called endometriosis.Since at least 10% of women have endometriosis, it’s one of the most common diseases worldwide -- even more common than HIV/AIDS and cancer. In addition to affecting the lining of the pelvis, endometriosis may also affect one or more of the pelvic organs, including the uterus, fallopian tubes, ovaries, bowel, and bladder.
Endometriosis may cause the formation of large ovarian “chocolate” cysts (endometriomas), pelvic adhesions and scarring, infertility, and bowel and bladder dysfunction. Sometimes, it may even invade the bladder, bowel, and other pelvic structures, causing severe complications.
What are the symptoms of endometriosis?
Pain is the main symptom of endometriosis, and women often experience chronic pelvic pain, painful periods, and/or painful intercourse. Pain is perceived by the brain when endometriosis invades the nerves that supply the pelvis.Prostaglandin activity in the uterus also aggravates deposits of endometriosis in the abdomen and pelvis causing significant pain. Ultimately, estrogen promotes the growth and expansion of endometriosis. Therefore, the mainstay of treatment is aimed at counteracting or eliminating the effects of estrogen and prostaglandins.
How is endometriosis treated?
Conservative treatment of endometriosis should be attempted first, and surgery is the last resort after exhausting conservative options. One minimally invasive surgical option is laparoscopic excision of endometriosis and the pelvic adhesions it may form.If pelvic adhesions are severe and involve the bowel or bladder, additional procedures may be necessary. Sometimes your surgeon might request assistance from a urologist or colorectal surgeon.
A urologist can place illuminating ureteral stents to aid in identification of the ureters and decrease the risk of injury. A colorectal surgeon can perform a proctosigmoidoscopy and possible bowel surgery. Laparoscopic excision or laser ablation of endometriosis is the recommended approach if the patient wishes to preserve her ability to get pregnant.
If conservative surgery is unsuccessful or future pregnancy is not desired, then the definitive solution is a hysterectomy. Removal of solely the uterus significantly reduces prostaglandin activity, which in turn considerably diminishes aggravation of endometriosis. Thus, the ovaries can usually be preserved preventing undesirable, sometimes debilitating, menopausal symptoms.
Abdominal hysterectomy and vaginal hysterectomy are the standard of care and involve an overnight stay in the hospital. The definitive minimally-invasive solution is provided by outpatient laparoscopic hysterectomy or robotic hysterectomy.
Most cases at MIGS are performed laparoscopically. The advantages of a laparoscopic procedure are many. Patients usually go home the same day, the recovery time is faster and less painful, and the cosmetic outcome is better.

Fibroids
Fibroids can be present in your uterus without you being aware of them, but for some women, they do cause heavy periods and cramping. If you have symptomatic fibroids, Nathan Mordel, MD, and the team at Wellstar Minimally Invasive Gynecological Surgery provide cutting-edge treatments to resolve the problem. They use the latest medical technologies and surgical techniques to treat fibroids and are experts in performing procedures such as hysteroscopic myomectomy, robotically assisted using laparoscopic and robotic myomectomy, or hysterectomy.
What are fibroids?
Fibroids, also known as leiomyomas, are benign tumors originating from uterine tissue. They can vary greatly in size and number. Symptoms and treatment options are affected by the size, number, and location of the leiomyomas.Since fibroids are very common and most of the time they don’t cause bothersome symptoms, they go undetected. However, some studies report leiomyomas in more than half of women by age 50.
While the majority of women usually have no symptoms, 1 in 4 women ends up with symptoms severe enough to require treatment. Symptomatic patients may experience heavy bleeding, irregular bleeding, and painful periods, as well as pelvic pressure and urinary frequency from an enlarged uterus.
How are fibroids treated?
If conservative options are unsuccessful, contraindicated, or not desired, then surgery is offered. For patients with fibroid tumors who wish to have children, a myomectomy is a possible option.Myomectomy is a surgical procedure that removes only the fibroid tumors from the uterus. If incisions are made into the uterine wall, then they are closed with sutures and the uterus is left intact. There are a variety of ways this procedure can be performed, and the approach depends on the number, location, and size of the fibroids.
Hysteroscopic myomectomy involves placing a hysteroscope into the uterus via the vaginal canal and removing small submucosal fibroids.
Robotically assisted laparoscopic myomectomy is a minimally invasive approach to removing fibroids and is the preferred method at Wellstar Minimally Invasive Gynecological Surgery.
Uterine fibroid embolization (UFE) performed by an interventional radiologist, is also used to treat symptomatic fibroids, though it's not advised for women wishing to preserve fertility.
Patients who completed their childbearing may choose robotically assisted laparoscopic hysterectomy, which is the ultimate method to treated symptomatic fibroids.
The advantages of a laparoscopic procedure are many. Patients usually go home the same day, the recovery time is faster and less painful, cosmetic outcome is better and many complications are virtually eliminated.

Robotic Hysterectomy
Finding out you need to undergo a hysterectomy is a scary thought because a hysterectomy sounds like a major procedure. However, Nathan Mordel, MD, and the team at Wellstar Minimally Invasive Gynecological Surgery use advanced robotic technology to carry out minimally invasive hysterectomies. Most women can have this surgery as outpatients and return to normal life far more quickly than they might expect.
What is robotic hysterectomy?
There are a variety of ways a hysterectomy procedure can be performed (in the absence of cancer) and the approach depends on the size of the uterus, the patient’s history of previous abdominal surgeries, and indications for the procedure, as well as the surgeon’s level of skill and comfort. Abdominal hysterectomy and vaginal hysterectomy are the standard of care and involve up to two nights in the hospital. The definitive minimally-invasive solution is provided by outpatient laparoscopic hysterectomy or robotic hysterectomy. Most of the cases seen at Wellstar Minimally Invasive Gynecological Surgery are performed laparoscopically, even when the uterus is very large. Robot-assisted surgery is the most advanced method of carrying out laparoscopic hysterectomy.
How is robotic hysterectomy carried out?
You undergo robotic hysterectomy under general anesthesia, so you’ll be asleep throughout the procedure. Your gynecologist operates using the da Vinci® Surgical System from a surgeon console using computer technology and a live camera feed to guide the robot. The camera relays a 3D, high-definition view of the inside of your body, magnified to enable your surgeon to make precise incisions. The da Vinci robot receives information in real-time from the surgeon console, performing the exact actions of the surgeon but with a precision not possible by hand. Using robot-assisted laparoscopic hysterectomy, it’s possible to remove your uterus through four tiny incisions, each ¼-½ of an inch long.
What are the advantages of robotic hysterectomy?
Robotic technology enables gynecologists to perform the most precise, minimally invasive hysterectomy available today. For most women, hysterectomy using the da Vinci system offers many benefits over traditional open surgery, including:
- Significantly less pain
- Minimal blood loss
- No need for transfusion
- Fewer complications
- Shorter hospital stay
- Quicker recovery and return to normal activities
- Minimal scarring
- Better outcomes
- Improved patient satisfaction

Robotic Myomectomy
Myomectomy is a procedure that removes uterine fibroids when they’re causing unpleasant symptoms such as excessive bleeding and cramping. Nathan Mordel, MD, and the team at Wellstar Minimally Invasive Gynecological Surgery use advanced robotic technology to carry out minimally invasive myomectomies, minimizing tissue damage and ensuring a speedier recovery than you’d experience with open surgery. Find out more by calling Wellstar Minimally Invasive Gynecological Surgery or book an appointment online.Why might I need robotic myomectomy surgery?
You might need robotic myomectomy if you have uterine fibroids, benign growths within the tissues lining your uterus. Fibroids could be very small and cause no symptoms at all, or they can grow to such a size that they make your abdomen swell. You can have one, a few, or numerous fibroids, and they could be a mixture of different sizes. Many women don’t experience any problems because of fibroids, but they can cause severe pain and heavy bleeding during menstruation.What is robotic myomectomy?
Robotic myomectomy is a minimally invasive approach to removing fibroids from your uterus so you don’t need to undergo open surgery. The highly experienced gynecologists at Wellstar Minimally Invasive Gynecological Surgery specialize in robotic procedures, including robot-assisted myomectomy. The procedure involves making five tiny incisions ranging from ¼ to ½ inches into your abdomen. Through these incisions, your surgeon can remove fibroid material using the da Vinci® Surgical System. Your gynecologist controls the robot using a surgeon console, guiding the robotic arms to make the incisions and extract the fibroids. The robot is performing the surgery but under the total control of your surgeon at all times.Is robotic myomectomy right for me?
If you have uterine fibroids that are causing you pain and difficult menstruation, there are a number of treatments available. Once your work-up is complete and cancer has been ruled out, conservative treatment should typically be attempted first. First-line therapy is prescribing a hormonal agent if no contraindications exist. Hormonal agents may contain either a combination of an estrogen and a progestin medication or may contain a progestin-only compound. Choices include:- Birth control pills
- Vaginal rings
- Transdermal patches
- Intrauterine devices (IUDs)
- Injection progesterone
Usually, the therapeutic impact only lasts as long as these agents are given. If pelvic pain occurs along with abnormal bleeding, nonsteroidal anti-inflammatory medications are usually given as well.
If conservative hormonal treatments are contraindicated or unsuccessful, then usually a minimally invasive option is offered next. For small submucosal fibroids (ones inside the uterine cavity) and uterine polyps, an operative hysteroscopy is offered.
Uterine endometrial ablation is one of the most effective options for symptomatic small fibroids. The procedure is designed for patients who don’t desire future pregnancies and prefer not to have surgery.
Endometrial ablation is an excellent alternative to hysterectomy for appropriate candidates. There are no hormones or surgery involved. Endometrial ablation destroys the lining of the uterus by using either a freezing (cryoablation) or heat energy (thermal ablation) technique.
If none of these treatments proves effective, your surgeon can discuss the surgical options with you. These include:
- Hysteroscopic myomectomy
- Abdominal myomectomy
- Laparoscopic or robotic myomectomy

Laparoscopic Hysterectomy
What is a laparoscopic hysterectomy?
Total laparoscopic hysterectomy (TLH) requires general anesthesia and vaginal and laparoscopic incisions to remove the uterus and cervix. The important difference is that in TLH vaginal retractors are not needed since the vagina is closed by suturing from inside the pelvic cavity under direct vision of the laparoscope (camera).This procedure is technically more difficult than TAH (total abdominal hysterectomy), TVH (total vaginal hysterectomy), LAVH (laparoscopically assisted vaginal hysterectomy), and LSH (laparoscopic supracervical hysterectomy) since it requires the surgeon to be trained in advanced laparoscopy. Special energy sources are used to seal and divide the blood vessels and to detach the uterus from its attachments.
If the uterus is small, it’s removed through the vagina. If the uterus is large, a special device called a morcellator is used to cut the uterus into small strips so it can be removed through the incision site. Usually, TLH is an outpatient surgery, and patients typically go home 6-8 hours after surgery. Postoperative recovery is normally 2-3 weeks and patients can usually resume intercourse after six weeks.
What are the benefits of laparoscopic hysterectomy?
The benefits of laparoscopic surgery are many. To name a few, patients usually go home the same day, the recovery time is faster and less painful, and the cosmetic outcome is better.At Wellstar, the surgeons are trained in advanced laparoscopy and perform the overwhelming majority of their cases laparoscopically, even in patients that have a very large uterus or have had multiple abdominal surgeries in the past. They feel that the minimally invasive laparoscopic approach to removing the uterus is the best approach for the patient.
What is laparoscopic supracervical hysterectomy?
LSH requires general anesthesia and only laparoscopic incisions to remove the uterus. The cervix is spared thus there is no vaginal incision needed. The LSH procedure is essentially sutureless and bloodless since special energy sources are used to seal and divide the blood vessels and to detach the uterus from the cervix and ovaries.The uterus is removed through the belly button incision site. Having performed over 1500 laparoscopic supracervical hysterectomy procedures, Dr. Mordel notes that LSH avoids unpleasant scars and shortening the vagina, eliminates the need for retractors and bowel packing, and significantly reduces hospital stays, postoperative pain, and recovery time.
LSH generates less pain than any other hysterectomy. It is usually an outpatient procedure, and patients typically go home 6-8 hours after surgery and return to normal activities in about two weeks.
Preservation of the cervix maintains the integrity of the vagina so it does not become shortened. It also saves some of the blood supply and nerve network and therefore may preserve pelvic floor function, including sexual response. However, this is not proven in the literature.
After having a procedure where the cervix is spared, a patient will need to have routine Pap tests since the risk of cervical cancer still exists. Also, patients should be aware that there is a very small possibility that occasional light vaginal spotting from the cervix can occur.


